EMP1, a novel poor prognostic factor in pediatric leukemia regulates prednisolone resistance, cell proliferation, migration and adhesion.
Ariës, IM; Jerchel, IS; van den Dungen, RE; van den Berk, LC; Boer, JM; Horstmann, MA; Escherich, G; Pieters, R; den Boer, ML
Leukemia
2014
Show Abstract
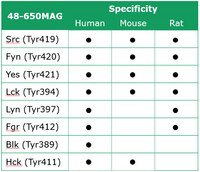
Still 20% of pediatric acute lymphoblastic leukemia (ALL) patients relapse on or after current treatment strategies. Treatment failure is associated with resistance to prednisolone. We aimed to find new druggable targets that modulate prednisolone resistance. We generated microarray gene expression profiles of 256 pediatric ALL patient samples and identified a 3.4-fold increase in epithelial membrane protein 1 (EMP1) expression in in vitro prednisolone-resistant compared with -sensitive patients (P=0.003). EMP1 silencing in six precursor-B ALL (BCP-ALL) and T-ALL cell lines induced apoptosis and cell-cycle arrest leading to 84.1±4.5% reduction in survival compared with non-silencing control transduced cells (non-silencing control short hairpin, shNSC) (P=0.014). Moreover, EMP1 silencing sensitized to prednisolone up to 18.8-fold (P<0.001). EMP1 silencing also abrogated migration and adhesion to mesenchymal stromal cells (MSCs) by 78.3±9.0 and 29.3±4.1% compared with shNSC (P<0.05). We discovered that EMP1 contributes to MSC-mediated prednisolone resistance. Pathway analysis indicated that EMP1 signals through the Src kinase family. EMP1-high BCP-ALL patients showed a poorer 5-year event-free survival compared with EMP1-low patients (77±2 vs 89±2%, P=0.003). Multivariate analysis taking along white blood cell count, age, prednisolone resistance and subtype identified EMP1 as an independent predictor for poor outcome in BCP-ALL (P=0.004, hazard ratio: 2.36 (1.31-4.25). This study provides preclinical evidence that EMP1 is an interesting candidate for drug development to optimize treatment of BCP-ALL.Leukemia advance online publication, 14 March 2014; doi:10.1038/leu.2014.80. | 24625531
 |
TNF-like weak inducer of apoptosis (TWEAK) promotes glioblastoma cell chemotaxis via Lyn activation.
Dhruv, Harshil D, et al.
Carcinogenesis, (2013)
2013
Show Abstract
The long-term survival of patients with glioblastoma (GB) is compromised by the proclivity for local invasion into the surrounding normal brain, escaping surgical resection and contributing to therapeutic resistance. Tumor necrosis factor-like weak inducer of apoptosis (TWEAK), a member of the tumor necrosis factor superfamily, can stimulate glioma cell invasion via binding to fibroblast growth factor-inducible 14 (Fn14) and subsequent activation of the Rho GTPase family member Rac1. Here, we demonstrate that TWEAK acts as a chemotactic factor for glioma cells, a potential process for driving cell invasion into the surrounding brain tissue. TWEAK exposure induced the activation of Src-family kinases (SFK), and pharmacologic suppression of SFK activity inhibited TWEAK-induced chemotactic migration. We employed a multiplexed Luminex assay and identified Lyn as a candidate SFK activated by TWEAK. Depletion of Lyn suppressed TWEAK-induced chemotaxis and Rac1 activity. Furthermore, Lyn gene expression levels increase with primary glioma tumor grade and inversely correlate with patient survival. These results show that TWEAK-induced glioma cell chemotaxis is dependent upon Lyn kinase function, and thus, provides opportunities for therapeutic targeting of this deadly disease. | 23975833
 |
Lyn, a Src family kinase, regulates activation of epidermal growth factor receptors in lung adenocarcinoma cells.
Sutton, P; Borgia, JA; Bonomi, P; Plate, JM
Molecular cancer
12
76
2013
Show Abstract
Activation of receptors for growth factors on lung epithelial cells is essential for transformation into tumor cells, supporting their viability and proliferation. In most lung cancer patients, EGFR is constitutively activated without evidence of mutation. Defining mechanisms for constitutive activation of EGFR could elucidate additional targets for therapy of lung cancers.The approach was to identify lung cancer cell lines with constitutively activated EGFR and use systematic selection of inhibitors to evaluate their effects on specific EGFR phosphorylations and downstream signaling pathways. Interactions between receptors, kinases, and scaffolding proteins were investigated by co-immunoprecipitation plus Western blotting.The results revealed a dependence on Src family of tyrosine kinases for downstream signaling and cell growth. Lyn, a Src family kinase functional in normal and malignant B-lymphocytes, was a defining signal transducer required for EGFR signaling in Calu3 cell line. Src family kinase activation in turn, was dependent on PKCßII. Lyn and PKC exist in membrane complexes of RACK1 and in association with EGFR which pairs with other receptor partners. Silencing of Lyn expression with interfering siRNA decreased EGFR activation and cell viability.The importance of Src family kinases and PKCßII in the initiation of the EGFR signaling pathway in lung tumor cells was demonstrated. We conclude that phosphorylation of EGFR is mediated through PKCßII regulation of Lyn activation, and occurs in association with RACK1 and Cbp/PAG proteins. We suggest that protein complexes in cell membranes, including lipid rafts, may serve as novel targets for combination therapies with EGFR and Src Family Kinase inhibitors in lung cancer. | 23866081
 |
LKB1/STK11 inactivation leads to expansion of a prometastatic tumor subpopulation in melanoma.
Liu, Wenjin, et al.
Cancer Cell, 21: 751-64 (2012)
2011
Show Abstract
Germline mutations in LKB1 (STK11) are associated with the Peutz-Jeghers syndrome (PJS), which includes aberrant mucocutaneous pigmentation, and somatic LKB1 mutations occur in 10% of cutaneous melanoma. By somatically inactivating Lkb1 with K-Ras activation (±p53 loss) in murine melanocytes, we observed variably pigmented and highly metastatic melanoma with 100% penetrance. LKB1 deficiency resulted in increased phosphorylation of the SRC family kinase (SFK) YES, increased expression of WNT target genes, and expansion of a CD24(+) cell population, which showed increased metastatic behavior in vitro and in vivo relative to isogenic CD24(-) cells. These results suggest that LKB1 inactivation in the context of RAS activation facilitates metastasis by inducing an SFK-dependent expansion of a prometastatic, CD24(+) tumor subpopulation. | 22698401
 |















 Antibody[188709-ALL].jpg)

