Coating conditions matter to collagen matrix formation regarding von Willebrand factor and platelet binding.
Shlomit Mendelboum Raviv,Katalin Szekeres-Csiki,Attila Jenei,Janos Nagy,Boris Shenkman,Naphtali Savion,Jolan Harsfalvi
Thrombosis research
129
2011
Show Abstract
Von Willebrand factor (VWF) and platelet binding needs a uniform collagen matrix therefore we aimed to find an optimal condition for the preparation of human type-I and type-III collagen matrices. | 22056526
 |
Extracellular matrix expression by equine oral and limb fibroblasts in in vitro culture.
Emma J Watts,Michael T Rose
Research in veterinary science
92
2011
Show Abstract
Wounds on the limbs of horses are notoriously difficult to heal, with over production of TGFβ1 thought to be responsible for excessive scarring; in contrast, wounds in the oral cavity heal rapidly with minimal scarring. This experiment aimed to determine the effect of TGFβ1 on the production of mRNA and proteins for various extracellular matrix components by two equine fibroblast cell lines isolated from the oral mucosa and distal limb. Fibronectin mRNA was up-regulated by TGFβ1 in the limb but not the oral cells. TGFβ1 increased the ratio of mRNA for collagen types I-III for the oral cells only. mRNA expression for TGFβ receptors-I and -II was significantly lower in limb fibroblasts, and treatment of either cell line with TGFβ1 down-regulated mRNA expression for both receptors. These differences may account for the improved healing seen in oral wounds compared to the excessive scarring seen in limb wounds. | 21481430
 |
BMP12 and BMP13 gene transfer induce ligamentogenic differentiation in mesenchymal progenitor and anterior cruciate ligament cells.
Meike Haddad-Weber,Patrick Prager,Manuela Kunz,Lothar Seefried,Franz Jakob,Martha M Murray,Christopher H Evans,Ulrich Nöth,Andre F Steinert
Cytotherapy
12
2009
Show Abstract
To date there are only very few data available on the ligamentogenic differentiation capacity of mesenchymal stromal/progenitor cells (MSC) and anterior cruciate ligament (ACL) fibroblasts. | 20334610
 |
Simultaneous analysis of multiple serum proteins adhering to the surface of medical grade polydimethylsiloxane elastomers.
Aleksandar Backovic,Dolores Wolfram,Barbara Del-Frari,Hildegunde Piza,Lukas A Huber,Georg Wick
Journal of immunological methods
328
2007
Show Abstract
Although polydimethylsiloxane (PDMS, silicone) elastomers are presumed to be chemically inert and of negligible toxicity, they induce a prompt acute inflammatory response with subsequent fibrotic reactions. Since local inflammatory and fibrotic side effects are associated with the proteinaceous film on the surface of silicone implants, the process of protein adherence to silicone is of practical medical relevance, and interesting from theoretical, clinical and biotechnological perspectives. It is hypothesized that the systemic side effects resembling rheumatoid and other connective tissue diseases may be triggered by local immunological changes, but this functional relationship has yet to be defined. Because the proteinaceous film on the surface of silicone has been identified as a key player in the activation of host defense mechanisms, we propose a test system based on a proteomics screen to simultaneously identify proteins adsorbed from serum to the surface of silicone. Herein, we describe protein adsorption kinetics on the surface of silicone implants, correlate the adhesion properties of serum proteins with the occurrence of adverse reactions to silicone, and successfully discriminate their signature on the silicone surface in a blinded study of patients suffering from fibrotic reactions (as determined by Baker scale) to silicone implants. | 17920619
 |
Peripheral nerve extracellular matrix remodeling in Charcot-Marie-Tooth type I disease.
Camilla Palumbo, Roberto Massa, Maria Beatrice Panico, Antonio Di Muzio, Paola Sinibaldi, Giorgio Bernardi, Andrea Modesti
Acta neuropathologica
104
287-96
2002
Show Abstract
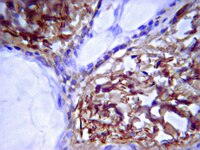
Charcot-Marie-Tooth type 1 disease (CMT1) is a group of inherited demyelinating neuropathies caused by mutations in genes expressed by myelinating Schwann cells. Rather than demyelination per se, alterations of Schwann cell-axon interactions have been suggested as the main cause of motor-sensory impairment in CMT1 patients. In an attempt to identify molecules that may be involved in such altered interactions, the extracellular matrix (ECM) remodeling occurring in CMT1 sural nerves was studied. For comparison, both normal sural nerves and sural nerves affected by neuropathies of different origin were used. The study was performed by immunohistochemical analysis using antibodies against collagen types I, III, IV, V, and VI and the glycoproteins fibronectin, laminin, vitronectin and tenascin. Up-regulation of collagens, fibronectin and laminin was commonly found in nerve biopsy specimens from patients affected by CMT1 and control diseases, but higher levels of overexpression were usually observed in CMT1 cases. On the other hand, vitronectin and tenascin appeared preferentially induced in CMT1 compared to other pathologies investigated here. Vitronectin, whose expression in normal nerves was limited to perineurial layers and to the walls of epineurial and endoneurial vessels, became strongly and diffusely expressed in the endoneurium in most CMT1 biopsy specimens. The expression of tenascin, confined to the perineurium, to vessel walls and to the nodes of Ranvier in normal nerves, was displaced and extended along the internodes of several nerve fibers in the majority of CMT1 nerves. Thus, compared with our pathological controls CMT1 seemed to determine the most extensive remodeling of peripheral nerve ECM. | 12172915
 |
Histological findings of surgically excised choroidal neovascular membranes after photodynamic therapy.
Schnurrbusch, U E, et al.
Br J Ophthalmol, 85: 1086-91 (2001)
2001
Show Abstract
AIM: To investigate effects of photodynamic therapy (PDT) on human choroidal neovascularisation (CNV). METHODS: Two patients with recurrences after PDT with verteporfin underwent surgical extraction of the CNV. Immediately after surgical excision the subfoveal neovascular membranes were divided for light microscopic and for electron microscopic processing. For light microscopy tissues were embedded in paraffin. Sections were stained with haematoxylin and eosin, and the periodic acid Schiff (PAS) reaction was performed to determine histological diagnosis and to ensure tissue quality. For electron microscopy the specimens were fixed in glutaraldehyde and embedded in epoxy resin. Semithin sections were stained with uranyl acetate and lead citrate and examined with a transmission electron microscope. RESULTS: Light microscopy showed thick fibrovascular membranes in both cases. On the outer surface remnants of retinal pigment epithelial cells resting on thickened inner aspect of Bruch's membrane were found. On the retinal side some outer segments were found. The membrane showed areas with irregularly shaped vessels. Electron photomicrographs showed occluded vessels within the CNV containing thrombotic masses and/or ultrastructural damage of the neovascular endothelium. Most of the vessels presented regressive changes with vacuolisation and fragmentation of the neovascular endothelium accompanied by disintegration of the endothelial cell layer. Extravasation of red blood cells was observed. Occasionally, vessels with normal endothelium containing intact red blood cells were observed. Some vessels contained immature endothelial cells. At some locations the retinal pigment epithelium cells (RPE) were metaplastic showing highly vacuolised cytoplasm. CONCLUSIONS: These findings suggest that the evidence of fluorescein leakage from the CNV and enlargement of the neovascular complex following PDT could be related to new vessel growth and recanalisation of occluded vessels. Additionally, RPE disturbances were observed in the specimens. This finding may be related to the original pathology or could indicate that PDT treatment may result in RPE atrophy. | 11520762
 |
Fibrocartilages in the extensor tendons of the interphalangeal joints of human toes
Milz, S, et al
Anat Rec, 252:264-70 (1998)
1998
| 9776080
 |
Fibrillin microfibrils are reduced in skin exhibiting striae distensae.
R E Watson, E J Parry, J D Humphries, C J Jones, D W Polson, C M Kielty, C E Griffiths, R E Watson, E J Parry, J D Humphries, C J Jones, D W Polson, C M Kielty, C E Griffiths
The British journal of dermatology
138
931-7
1998
Show Abstract
Striae distensae (striae: stretch marks) are a common disfiguring condition associated with continuous and progressive stretching of the skin--as occurs during pregnancy. The pathogenesis of striae is unknown but probably relates to changes in those structures that provide skin with its tensile strength and elasticity. Such structures are components of the extracellular matrix, including fibrillin, elastin and collagens. Using a variety of histological techniques, we assessed the distribution of these extracellular matrix components in skin affected by striae. Pregnant women were assessed for the presence of striae, and punch biopsies were obtained from lesional striae and adjacent normal skin. Biopsies were processed for electron microscopy, light microscopy and immunohistochemistry. For histological examination, 7 microns frozen sections were stained so as to identify the elastic fibre network and glycosaminoglycans. Biopsies were also examined with a panel of polyclonal antibodies against collagens I and III, and fibrillin and elastin. Ultrastructural analysis revealed alterations in the appearance of skin affected by striae compared with that of normal skin in that the dermal matrix of striae was looser and more floccular. Light microscopy revealed an increase in glycosaminoglycan content in striae. Furthermore, the number of vertical fibrillin fibres subjacent to the dermal-epidermal junction (DEJ) and elastin fibres in the papillary dermis was significantly reduced in striae compared with normal skin. The orientation of elastin and fibrillin fibres in the deep dermis showed realignment in that the fibres ran parallel to the DEJ. However, no significant alterations were observed in any other extracellular matrix components. This study identifies a reorganization and diminution of the elastic fibre network of skin affected by striae. Continuous strain on the dermal extracellular matrix, as occurs during pregnancy, may remodel the elastic fibre network in susceptible individuals and manifest clinically as striae distensae. | 9747352
 |
The fetal fibroblast: the effector cell of scarless fetal skin repair.
H P Lorenz, R Y Lin, M T Longaker, D J Whitby, N S Adzick
Plastic and reconstructive surgery
96
1251-9; discussion 1260-1
1994
Show Abstract
Human fetal skin heals without scar formation when it is transplanted to a subcutaneous location on an adult athymic mouse and subsequently wounded. In contrast, human fetal skin of identical gestational age heals with scar formation when transplanted to a cutaneous location on the athymic mouse recipient. To determine if mouse (adult) or human (fetal) fibroblasts are healing the graft wounds, we performed indirect immunohistochemistry for mouse and human collagen types I and III. Full-thickness skin grafts (n = 51) from human fetuses at 18 weeks' (n = 4) or 24 weeks' (n = 2) gestational age were placed onto athymic mice in two locations: cutaneously onto a fascial bed and subcutaneously in a pocket under the murine panniculus carnosus. Linear incisions were made in each graft 7 days after transplantation. Grafts were harvested at 7, 14, and 21 days after wounding and stained with hematoxylin and eosin or Mallory's trichrome. Immunohistochemistry for either human collagen type I or type III or for mouse collagen type I was performed. The subcutaneous grafts healed with human collagen types I and III in a scarless pattern. The wound collagen pattern was reticular and unrecognizable from the surrounding dermis. Hair follicles and sebaceous gland patterns were unchanged in the wounded dermis. Conversely, the cutaneous grafts healed with mouse collagen in a scar pattern with disorganized collagen fibers and no appendages. Mouse collagen scar was present along the base of the cutaneous grafts and as a thin capsule around the subcutaneous grafts. We conclude that (1) subcutaneous grafts heal with human fetal collagen and no scar formation, and (2) cutaneous grafts heal with mouse collagen in a scar pattern. Fetal fibroblasts can heal fetal skin wounds without scar despite being perfused by adult serum and inflammatory cells in an adult environment. These data suggest that the fetal fibroblast is the major effector cell for scarless fetal skin repair. | 7480221
 |
Chronic hibernating myocardium: interstitial changes.
J Ausma, J Cleutjens, F Thoné, W Flameng, F Ramaekers, M Borgers
Molecular and cellular biochemistry
147
35-42
1994
Show Abstract
Chronic left ventricular dysfunctional but viable myocardium of patients with chronic hibernation is characterized by structural changes, which consist of depletion of contractile elements, accumulation of glycogen, nuclear chromatin dispersion, depletion of sarcoplasmic reticulum and mitochondrial shape changes. These alterations are not reminiscent of degeneration but are interpreted as de-differentiation of the cardiomyocytes. The above mentioned changes are accompanied by a marked increase in the interstitial space. The present study describes qualitative and quantitative changes in the cellular and non-cellular compartments of the interstitial space. In chronic hibernating myocardial segments the increased extracellular matrix is filled with large amounts of type I collagen, type III collagen and fibronectin. An increase in the number of vimentin-positive cells (endothelial cells and fibroblasts) compared with normal myocardium is seen throughout the extracellular matrix. The increase in interstitial tissue is considered as one of the main determinants responsible for the lack of immediate recovery of contractile function after restoration of the blood flow to the affected myocardial segments of patients with chronic left ventricular dysfunction. | 7494552
 |