Dental pulp stem cells: a new cellular resource for corneal stromal regeneration.
Syed-Picard, FN; Du, Y; Lathrop, KL; Mann, MM; Funderburgh, ML; Funderburgh, JL
Stem cells translational medicine
4
276-85
2015
Zobrazit abstrakt
Corneal blindness afflicts millions of individuals worldwide and is currently treated by grafting with cadaveric tissues; however, there are worldwide donor tissue shortages, and many allogeneic grafts are eventually rejected. Autologous stem cells present a prospect for personalized regenerative medicine and an alternative to cadaveric tissue grafts. Dental pulp contains a population of adult stem cells and, similar to corneal stroma, develops embryonically from the cranial neural crest. We report that adult dental pulp cells (DPCs) isolated from third molars have the capability to differentiate into keratocytes, cells of the corneal stoma. After inducing differentiation in vitro, DPCs expressed molecules characteristic of keratocytes, keratocan, and keratan sulfate proteoglycans at both the gene and the protein levels. DPCs cultured on aligned nanofiber substrates generated tissue-engineered, corneal stromal-like constructs, recapitulating the tightly packed, aligned, parallel fibrillar collagen of native stromal tissue. After injection in vivo into mouse corneal stroma, human DPCs produced corneal stromal extracellular matrix containing human type I collagen and keratocan and did not affect corneal transparency or induce immunological rejection. These findings demonstrate a potential for the clinical application of DPCs in cellular or tissue engineering therapies for corneal stromal blindness. | | | 25713466
 |
Human endometrial mesenchymal stem cells modulate the tissue response and mechanical behavior of polyamide mesh implants for pelvic organ prolapse repair.
Ulrich, D; Edwards, SL; Su, K; Tan, KS; White, JF; Ramshaw, JA; Lo, C; Rosamilia, A; Werkmeister, JA; Gargett, CE
Tissue engineering. Part A
20
785-98
2014
Zobrazit abstrakt
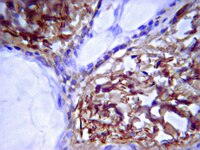
Pelvic organ prolapse (POP) is defined as the descent of one or more of the pelvic structures into the vagina and includes uterine, vaginal vault, and anterior or posterior vaginal wall prolapse. The treatment of POP may include implantation of a synthetic mesh. However, the long-term benefit of mesh surgery is controversial due to complications such as mesh exposure or pain. The aim of this study was to use a tissue engineering (TE) approach to assess the in vivo biological and biomechanical behavior of a new gelatin/polyamide mesh, seeded with a novel source of mesenchymal stem cells in a subcutaneous rat model of wound repair.W5C5-enriched human endometrial mesenchymal stem cells (eMSC) were seeded onto meshes (gelatin-coated polyamide knit) at 100,000 cells/cm². Meshes, with or without cells were subcutaneously implanted dorsally in immunocompromised rats for 7, 30, 60, and 90 days. Flow cytometry was used to detect DiO labeled cells after explantation. Immunohistochemical assessment of foreign body reaction and tissue integration were conducted. Total collagen and the levels of collagens type III and type I were determined. Uniaxial tensiometry was performed on explanted meshes, originally seeded with and without cells, at days 7 and 90.Implanted meshes were well tolerated, with labeled cells detected on the mesh up to 14 days postimplantation. Meshes with cells promoted significantly more neovascularization at 7 days (pless than 0.05) and attracted fewer macrophages at 90 days (pless than 0.05). Similarly, leukocyte infiltration was significantly lower in the cell-seeded meshes at 90 days (pless than 0.05). Meshes with cells were generally less stiff than those without cells, after 7 and 90 days implantation.The TE approach used in this study significantly reduced the number of inflammatory cells around the implanted mesh and promoted neovascularization. Seeding with eMSC exerts an anti-inflammatory effect and promotes wound repair with new tissue growth and minimal fibrosis, and produces mesh with greater extensibility. Cell seeding onto polyamide/gelatin mesh improves mesh biocompatibility and may be an alternative option for future treatment of POP. | | | 24083684
 |
Thrombin induces epithelial-mesenchymal transition and collagen production by retinal pigment epithelial cells via autocrine PDGF-receptor signaling.
Bastiaans, J; van Meurs, JC; van Holten-Neelen, C; Nagtzaam, NM; van Hagen, PM; Chambers, RC; Hooijkaas, H; Dik, WA
Investigative ophthalmology & visual science
54
8306-14
2013
Zobrazit abstrakt
De-differentiation of RPE cells into mesenchymal cells (epithelial-mesenchymal transition; EMT) and associated collagen production contributes to development of proliferative vitreoretinopathy (PVR). In patients with PVR, intraocular coagulation cascade activation occurs and may play an important initiating role. Therefore, we examined the effect of the coagulation proteins factor Xa and thrombin on EMT and collagen production by RPE cells.Retinal pigment epithelial cells were stimulated with factor Xa or thrombin and the effect on zonula occludens (ZO)-1, α-smooth muscle actin (α-SMA), collagen, and platelet-derived growth factor (PDGF)-B were determined by real-time quantitative-polymerase chain reaction (RQ-PCR), immunofluorescence microscopy, and HPLC and ELISA for collagen and PDGF-BB in culture supernatants, respectively. PDGF-receptor activation was determined by phosphorylation analysis and inhibition studies using the PDGF-receptor tyrosine kinase inhibitor AG1296.Thrombin reduced ZO-1 gene expression (P less than 0.05) and enhanced expression of the genes encoding α-SMA and the pro-alpha1 chain of collagen type-1 (P less than 0.05), indicating EMT. Also, ZO-1 protein expression declined on thrombin stimulation, whereas production of α-SMA and collagen increased. In contrast to thrombin, factor Xa hardly stimulated EMT by RPE. Thrombin clearly induced PDGF-BB production and PDGF-Rβ chain phosphorylation in RPE. Moreover, AG1296 significantly blocked the effect of thrombin on EMT and collagen production.Our findings demonstrate that thrombin is a potent inducer of EMT by RPE via autocrine activation of PDGF-receptor signaling. Coagulation cascade-induced EMT of RPE may thus contribute to the formation of fibrotic retinal membranes in PVR and should be considered as treatment target in PVR. | | | 24302586
 |
Isolation and characterization of novel, highly proliferative human CD34/CD73-double-positive testis-derived stem cells for cell therapy.
Choi, WY; Jeon, HG; Chung, Y; Lim, JJ; Shin, DH; Kim, JM; Ki, BS; Song, SH; Choi, SJ; Park, KH; Shim, SH; Moon, J; Jung, SJ; Kang, HM; Park, S; Chung, HM; Ko, JJ; Cha, KY; Yoon, TK; Kim, H; Lee, DR
Stem cells and development
22
2158-73
2013
Zobrazit abstrakt
Human adult stem cells are a readily available multipotent cell source that can be used in regenerative medicine. Despite many advantages, including low tumorigenicity, their rapid senescence and limited plasticity have curtailed their use in cell-based therapies. In this study, we isolated CD34/CD73-double-positive (CD34(+)/CD73(+)) testicular stromal cells (HTSCs) and found that the expression of CD34 was closely related to the cells' stemness and proliferation. The CD34(+)/CD73(+) cells grew in vitro for an extended period of time, yielding a multitude of cells (5.6×10(16) cells) without forming tumors in vivo. They also differentiated into all three germ layer lineages both in vitro and in vivo, produced cartilage more efficiently compared to bone marrow stem cells and, importantly, restored erectile function in a cavernous nerve crush injury rat model. Thus, these HTSCs may represent a promising new autologous cell source for clinical use. | | | 23509942
 |
Oxygen tension is a determinant of the matrix-forming phenotype of cultured human meniscal fibrochondrocytes.
Adesida, AB; Mulet-Sierra, A; Laouar, L; Jomha, NM
PloS one
7
e39339
2011
Zobrazit abstrakt
Meniscal cartilage displays a poor repair capacity, especially when injury is located in the avascular region of the tissue. Cell-based tissue engineering strategies to generate functional meniscus substitutes is a promising approach to treat meniscus injuries. Meniscus fibrochondrocytes (MFC) can be used in this approach. However, MFC are unable to retain their phenotype when expanded in culture. In this study, we explored the effect of oxygen tension on MFC expansion and on their matrix-forming phenotype.MFC were isolated from human menisci followed by basic fibroblast growth factor (FGF-2) mediated cell expansion in monolayer culture under normoxia (21%O(2)) or hypoxia (3%O(2)). Normoxia and hypoxia expanded MFC were seeded on to a collagen scaffold. The MFC seeded scaffolds (constructs) were cultured in a serum free chondrogenic medium for 3 weeks under normoxia and hypoxia. Constructs containing normoxia-expanded MFC were subsequently cultured under normoxia while those formed from hypoxia-expanded MFC were subsequently cultured under hypoxia. After 3 weeks of in vitro culture, the constructs were assessed biochemically, histologically and for gene expression via real-time reverse transcription-PCR assays. The results showed that constructs under normoxia produced a matrix with enhanced mRNA ratio (3.5-fold higher; pless than 0.001) of collagen type II to I. This was confirmed by enhanced deposition of collagen II using immuno-histochemistry. Furthermore, the constructs under hypoxia produced a matrix with higher mRNA ratio of aggrecan to versican (3.5-fold, pless than 0.05). However, both constructs had the same capacity to produce a glycosaminoglycan (GAG) -specific extracellular matrix.Our data provide evidence that oxygen tension is a key player in determining the matrix phenotype of cultured MFC. These findings suggest that the use of normal and low oxygen tension during MFC expansion and subsequent neo-tissue formation cultures may be important in engineering different regions of the meniscus. | | | 22720095
 |
Hypoxia mediated isolation and expansion enhances the chondrogenic capacity of bone marrow mesenchymal stromal cells.
Adesida, AB; Mulet-Sierra, A; Jomha, NM
Stem cell research & therapy
3
9
2011
Zobrazit abstrakt
The capacity of bone marrow mesenchymal stromal cells (BMSCs) to be induced into chondrocytes has drawn much attention for cell-based cartilage repair. BMSCs represent a small proportion of cells of the bone marrow stromal compartment and, thus, culture expansion is a necessity for therapeutic use. However, there is no consensus on how BMSCs should be isolated nor expanded to maximize their chondrogenic potential. During embryonic development pluripotent stem cells differentiate into chondrocytes and form cartilage in a hypoxic microenvironment.Freshly harvested human BMSCs were isolated and expanded from the aspirates of six donors, under either hypoxic conditions (3% O2) or normoxic conditions (21% O2). A colony-forming unit fibroblastic (Cfu-f) assay was used to determine the number of cell colonies developed from each donor. BMSCs at passage 2 (P2) were characterized by flow cytometry for the phenotypic expression of cell surface markers on mesenchymal stem cells. BMSCs at P2 were subsequently cultured in vitro as three-dimensional cell pellets in a defined serum-free chondrogenic medium under normoxic and hypoxic conditions. Chondrogenic differentiation of the BMSCs was characterized by biochemical and histological methods and by quantitative gene-expression analysis.After 14 days of culture, the number of BMSC colonies developed under hypoxia was generally higher (8% to 38% depending on donor) than under normoxia. BMSCs were positive for the cell surface markers CD13, CD29, CD44, CD73, CD90, CD105 and CD151, and negative for CD34. Regardless of the oxygen tension during pellet culture, hypoxia-expanded BMSC pellets underwent a more robust chondrogenesis than normoxia-expanded BMSC pellets after three weeks of culture, as judged by increased glycosaminoglycan synthesis and Safranin O staining, along with increased mRNA expression of aggrecan, collagen II and Sox9. Hypoxic conditions enhanced the mRNA expression of hypoxia inducible factor-2 alpha (HIF-2α) but suppressed the mRNA expression of collagen X in BMSC pellet cultures regardless of the oxygen tension during BMSC isolation and propagation.Taken together, our data demonstrate that isolation and expansion of BMSCs under hypoxic conditions augments the chondrogenic potential of BMSCs. This suggests that hypoxia-mediated isolation and expansion of BMSCs may improve clinical applications of BMSCs for cartilage repair. | | | 22385573
 |
Neuregulin induces CTGF expression in hypertrophic scarring fibroblasts.
Jun-Sub Kim,Ihn-Geun Choi,Boung-Chul Lee,Jae-Bong Park,Jin-Hee Kim,Je Hoon Jeong,Ji Hoon Jeong,Cheong Hoon Seo
Molecular and cellular biochemistry
365
2011
Zobrazit abstrakt
Hypertrophic scarring (HTS) is a common fibroproliferative disorder that typically follows thermal and other injuries involving the deep dermis. These pathogenic mechanisms are regulated by connective tissue growth factor (CTGF) and transforming growth factor-β. We found that neuregulin-1 (NRG1), as well as NRG receptors, HER-2, and HER-3 were upregulated in HTS fibroblasts (HTSF), compared with normal fibroblasts. Furthermore, NRG1 stimulation increased the expression of CTGF in HTSF. In the presence of inhibitors of PI3K, Src, Smad, or reactive oxygen species, the effect of NRG1 on CTGF expression decreased significantly. In particular, the combination of LY294002 or PP2 with SB431542 blocked NRG1-mediated CTGF expression in HTSF. Finally, we demonstrated that siRNA for CTGF, AG825, LY294002, and PP2, either alone or in co-treatment, effectively reduced extracellular matrix expression. Taken together, our results suggest that NRG1 is involved in fibrotic scar pathogenesis via PI3K- or Src-mediated CTGF expression. | | | 22350758
 |
Decreased hypertrophic differentiation accompanies enhanced matrix formation in co-cultures of outer meniscus cells with bone marrow mesenchymal stromal cells.
Saliken, DJ; Mulet-Sierra, A; Jomha, NM; Adesida, AB
Arthritis research & therapy
14
R153
2011
Zobrazit abstrakt
The main objective of this study was to determine whether meniscus cells from the outer (MCO) and inner (MCI) regions of the meniscus interact similarly to or differently with mesenchymal stromal stem cells (MSCs). Previous study had shown that co-culture of meniscus cells with bone marrow-derived MSCs result in enhanced matrix formation relative to mono-cultures of meniscus cells and MSCs. However, the study did not examine if cells from the different regions of the meniscus interacted similarly to or differently with MSCs.Human menisci were harvested from four patients undergoing total knee replacements. Tissue from the outer and inner regions represented pieces taken from one third and two thirds of the radial distance of the meniscus, respectively. Meniscus cells were released from the menisci after collagenase treatment. Bone marrow MSCs were obtained from the iliac crest of two patients after plastic adherence and in vitro culture until passage 2. Primary meniscus cells from the outer (MCO) or inner (MCI) regions of the meniscus were co-cultured with MSCs in three-dimensional (3D) pellet cultures at 1:3 ratio, respectively, for 3 weeks in the presence of serum-free chondrogenic medium containing TGF-β1. Mono-cultures of MCO, MCI and MSCs served as experimental control groups. The tissue formed after 3 weeks was assessed biochemically, histochemically and by quantitative RT-PCR.Co-culture of inner (MCI) or outer (MCO) meniscus cells with MSCs resulted in neo-tissue with increased (up to 2.2-fold) proteoglycan (GAG) matrix content relative to tissues formed from mono-cultures of MSCs, MCI and MCO. Co-cultures of MCI or MCO with MSCs produced the same amount of matrix in the tissue formed. However, the expression level of aggrecan was highest in mono-cultures of MSCs but similar in the other four groups. The DNA content of the tissues from co-cultured cells was not statistically different from tissues formed from mono-cultures of MSCs, MCI and MCO. The expression of collagen I (COL1A2) mRNA increased in co-cultured cells relative to mono-cultures of MCO and MCI but not compared to MSC mono-cultures. Collagen II (COL2A1) mRNA expression increased significantly in co-cultures of both MCO and MCI with MSCs compared to their own controls (mono-cultures of MCO and MCI respectively) but only the co-cultures of MCO:MSCs were significantly increased compared to MSC control mono-cultures. Increased collagen II protein expression was visible by collagen II immuno-histochemistry. The mRNA expression level of Sox9 was similar in all pellet cultures. The expression of collagen × (COL10A1) mRNA was 2-fold higher in co-cultures of MCI:MSCs relative to co-cultures of MCO:MSCs. Additionally, other hypertrophic genes, MMP-13 and Indian Hedgehog (IHh), were highly expressed by 4-fold and 18-fold, respectively, in co-cultures of MCI:MSCs relative to co-cultures of MCO:MSCs.Co-culture of primary MCI or MCO with MSCs resulted in enhanced matrix formation. MCI and MCO increased matrix formation similarly after co-culture with MSCs. However, MCO was more potent than MCI in suppressing hypertrophic differentiation of MSCs. These findings suggest that meniscus cells from the outer-vascular regions of the meniscus can be supplemented with MSCs in order to engineer functional grafts to reconstruct inner-avascular meniscus. | | | 22726892
 |
Sliding contact loading enhances the tensile properties of mesenchymal stem cell-seeded hydrogels.
A H Huang,B M Baker,G A Ateshian,R L Mauck
European cells & materials
24
2011
Zobrazit abstrakt
The primary goal of cartilage tissue engineering is to recapitulate the functional properties and structural features of native articular cartilage. While there has been some success in generating near-native compressive properties, the tensile properties of cell-seeded constructs remain poor, and key features of cartilage, including inhomogeneity and anisotropy, are generally absent in these engineered constructs. Therefore, in an attempt to instill these hallmark properties of cartilage in engineered cell-seeded constructs, we designed and characterized a novel sliding contact bioreactor to recapitulate the mechanical stimuli arising from physiologic joint loading (two contacting cartilage layers). Finite element modeling of this bioreactor system showed that tensile strains were direction-dependent, while both tensile strains and fluid motion were depth-dependent and highest in the region closest to the contact surface. Short-term sliding contact of mesenchymal stem cell (MSC)-seeded agarose improved chondrogenic gene expression in a manner dependent on both the axial strain applied and transforming growth factor-β supplementation. Using the optimized loading parameters derived from these short-term studies, long-term sliding contact was applied to MSC-seeded agarose constructs for 21 d. After 21 d, sliding contact significantly improved the tensile properties of MSC-seeded constructs and elicited alterations in type II collagen and proteoglycan accumulation as a function of depth; staining for these matrix molecules showed intense localization in the surface regions. These findings point to the potential of sliding contact to produce engineered cartilage constructs that begin to recapitulate the complex mechanical features of the native tissue. | | | 22791371
 |
Fibroblast growth factor 2 enhances the kinetics of mesenchymal stem cell chondrogenesis.
Tiffany Cheng,Christina Yang,Norbert Weber,Hubert T Kim,Alfred C Kuo
Biochemical and biophysical research communications
426
2011
Zobrazit abstrakt
Treatment of mesenchymal stem cells (MSCs) with fibroblast growth factor 2 (FGF-2) during monolayer expansion leads to increased expression of cartilage-related molecules during subsequent pellet chondrogenesis. This may be due to faster differentiation and/or a durable change in phenotype. In order to evaluate changes over time, we assessed chondrogenesis of human MSCs at early and late time points during pellet culture using real-time PCR, measurement of glycosaminoglycan accumulation, and histology. Marked enhancement of chondrogenesis was seen early compared to controls. However, the differences from controls in gene expression dramatically diminished over time. Depending on conditions, increases in glycosaminoglycan accumulation were maintained. These results suggest that FGF-2 can enhance the kinetics of MSC chondrogenesis, leading to early differentiation, possibly by a priming mechanism. | | | 22982316
 |