Ω3 Supplementation and intermittent hypobaric hypoxia induce cardioprotection enhancing antioxidant mechanisms in adult rats.
Herrera, EA; Farías, JG; González-Candia, A; Short, SE; Carrasco-Pozo, C; Castillo, RL
Marine drugs
13
838-60
2015
Show Abstract
Intermittent hypobaric hypoxia (IH) is linked with oxidative stress, impairing cardiac function. However, early IH also activate cardio-protective mechanisms. Omega 3 fatty acids (Ω3) induce cardioprotection by reducing infarct size and reinforcing antioxidant defenses. The aim of this work was to determine the combined effects of IH and Ω3 on cardiac function; oxidative balance and inflammatory state. Twenty-eight rats were randomly divided into four groups: normobaric normoxia (N); N + Ω3 (0.3 g·kg-1·day-1); IH; and IH + Ω3. IH was induced by 4 intercalate periods of hypoxia (4 days)-normoxia (4 days) in a hypobaric chamber during 32 days. At the end of the exposure, hearts were mounted in a Langendorff system and subjected to 30 min of ischemia followed by 120 min of reperfusion. In addition, we determined HIF-1α and ATP levels, as well as oxidative stress by malondialdehyde and nitrotyrosine quantification. Further, the expression of the antioxidant enzymes superoxide dismutase, catalase, and glutathione peroxidase was determined. NF-kappaB and myeloperoxidase levels were assessed in the hearts. Relative to N hearts, IH improved left ventricular function (Left ventricular developed pressure: N; 21.8 ± 3.4 vs. IH; 42.8 ± 7.1 mmHg; p less than 0.05); reduced oxidative stress (Malondialdehyde: N; 14.4 ± 1.8 vs. IH; 7.3 ± 2.1 μmol/mg prot.; p less than 0.05); and increased antioxidant enzymes expression. Supplementation with Ω3 induces similar responses as IH group. Our findings suggest that both, IH and Ω3 in an independent manner, induce functional improvement by antioxidant and anti-inflammatory mechanisms, establishing cardio-protection. | | | 25658050
 |
Myofibrillar Ca(2+) sensitivity is uncoupled from troponin I phosphorylation in hypertrophic obstructive cardiomyopathy due to abnormal troponin T.
Bayliss, CR; Jacques, AM; Leung, MC; Ward, DG; Redwood, CS; Gallon, CE; Copeland, O; McKenna, WJ; Dos Remedios, C; Marston, SB; Messer, AE
Cardiovascular research
97
500-8
2013
Show Abstract
We studied the relationship between myofilament Ca(2+) sensitivity and troponin I (TnI) phosphorylation by protein kinase A at serines 22/23 in human heart troponin isolated from donor hearts and from myectomy samples from patients with hypertrophic obstructive cardiomyopathy (HOCM).We used a quantitative in vitro motility assay. With donor heart troponin, Ca(2+) sensitivity is two- to three-fold higher when TnI is unphosphorylated. In the myectomy samples from patients with HOCM, the mean level of TnI phosphorylation was low: 0.38 ± 0.19 mol Pi/mol TnI compared with 1.60 ± 0.19 mol Pi/mol TnI in donor hearts, but no difference in myofilament Ca(2+) sensitivity was observed. Thus, troponin regulation of thin filament Ca(2+) sensitivity is abnormal in HOCM hearts. HOCM troponin (0.29 mol Pi/mol TnI) was treated with protein kinase A to increase the level of phosphorylation to 1.56 mol Pi/mol TnI. No difference in EC(50) was found in thin filaments containing high and low TnI phosphorylation levels. This indicates that Ca(2+) sensitivity is uncoupled from TnI phosphorylation in HOCM heart troponin. Coupling could be restored by replacing endogenous troponin T (TnT) with the recombinant TnT T3 isoform. No difference in Ca(2+) sensitivity was observed if TnI was exchanged into HOCM heart troponin or if TnT was exchanged into the highly phosphorylated donor heart troponin. Comparison of donor and HOCM heart troponin by mass spectrometry and with adduct-specific antibodies did not show any differences in TnT isoform expression, phosphorylation or any post-translational modifications.An abnormality in TnT is responsible for uncoupling myofibrillar Ca(2+) sensitivity from TnI phosphorylation in the septum of HOCM patients. | | | 23097574
 |
Arginine and asymmetric dimethylarginine in puromycin aminonucleoside-induced chronic kidney disease in the rat.
Chen, GF; Moningka, NC; Sasser, JM; Zharikov, S; Cunningham, M; Tain, YL; Schwartz, IF; Baylis, C
American journal of nephrology
35
40-8
2012
Show Abstract
Reduced renal L-arginine (L-Arg) synthesis/transport, induction of arginases and increased endogenous NOS inhibitor, asymmetric dimethylarginine (ADMA) will inhibit NO production. This study investigated pathways of L-Arg synthesis/uptake/utilization, ADMA degradation and oxidant/antioxidants in puromycin aminonucleoside (PAN) chronic kidney disease (CKD).Rats were given low- (LD) or high-dose (HD) PAN and followed for 11 weeks for proteinuria. BP was measured and blood and tissues were harvested and analyzed for abundance of argininosuccinate synthase (ASS) and lyase (ASL), arginase, cationic amino acid transporter (CAT1) and dimethylargininedimethylaminohydrolase (DDAH) in kidney, cortex, aorta and liver. Arginase and DDAH activity, plasma L-Arg and ADMA, renal pathology and creatinine clearances were also measured.PAN caused dose-dependent kidney damage and hypertension and creatinine clearance fell in HD-PAN. Renal ASS fell in HD-PAN, renal cortex and aortic ASL and membrane CAT1 fell in both PAN groups. There was no activation of renal arginase, but aortic arginase increased in LD-PAN. Renal DDAH activity fell moderately in LD-PAN and markedly in HD-PAN where hepatic DDAH activity also fell. Plasma L-Arg was unchanged while ADMA rose moderately and dose-dependently with PAN. There were several indices of oxidative stress which was most prominent in HD-PAN.Reduction in renal ASS/ASL and loss of renal cortex CAT1 compromises renal L-Arg synthesis and release. Loss of aortic CAT1 impairs L-Arg uptake. Increased plasma ADMA was associated with progressive loss of renal DDAH activity. However, loss of renal clearance and falls in hepatic DDAH activity in HD-PAN did not have additive effects on plasma ADMA. | | | 22179117
 |
Nebivolol does not protect against 5/6 ablation/infarction induced chronic kidney disease in rats - comparison with angiotensin II receptor blockade.
Sasser, JM; Moningka, NC; Tsarova, T; Baylis, C
Life sciences
91
54-63
2012
Show Abstract
Nitric oxide (NO) deficiency contributes to chronic kidney disease progression. Nebivolol, a beta adrenergic receptor antagonist, may enhance endogenous NO. Here, we investigated whether Nebivolol attenuates hypertension and renal injury after 5/6 ablation/infarction (A/I). Efficacy was compared to the AT1 receptor antagonist Olmesartan.Kidney disease and hypertension were induced by right kidney ablation and ~2/3 infarction of the left kidney. Rats were treated orally with vehicle (placebo), Nebivolol (5mg/kg b.i.d.), or Olmesartan (2.5mg/kg/day) for 6 weeks after A/I.With placebo, glomerular sclerosis and tubulointersititial fibrosis developed with increased blood pressure and proteinuria, and a fall in NO(x) excretion. Olmesartan prevented these changes, but Nebivolol had no effect on these measures but lowered heart rate. Neither treatment reduced systemic oxidative stress (urinary hydrogen peroxide and TBARS). Compared to controls, renal cortex abundance of nNOSα decreased and nNOSβ increased in rats after 5/6 A/I, with no changes in eNOS. Neither treatment restored nNOSα; however, both reduced nNOSβ. Activity of DDAH was decreased by 5/6 A/I but restored by both treatments despite no increase in DDAH protein abundance. Kidney cortex abundance of manganese SOD fell after 5/6 A/I and was restored by treatment with Olmesartan but not Nebivolol. Extracellular and copper/zinc SOD abundances were not changed.In conclusion, Nebivolol showed no benefit after 6 weeks in rapidly progressing, ANG II-dependent 5/6 A/I model of chronic kidney disease. This contrasts to the protection seen with 6 month treatment of Nebivolol in the slowly progressing 5/6 ablation model. | Western Blotting | | 22727796
 |
Increased microparticle production and impaired microvascular endothelial function in aldosterone-salt-treated rats: protective effects of polyphenols.
López Andrés, N; Tesse, A; Regnault, V; Louis, H; Cattan, V; Thornton, SN; Labat, C; Kakou, A; Tual-Chalot, S; Faure, S; Challande, P; Osborne-Pellegrin, M; Martínez, MC; Lacolley, P; Andriantsitohaina, R
PloS one
7
e39235
2012
Show Abstract
We aimed to characterize circulating microparticles in association with arterial stiffness, inflammation and endothelial dysfunction in aldosterone-salt-induced hypertension in rats and to investigate the preventive effects of red wine polyphenols. Uninephrectomized male Sprague-Dawley rats were treated with aldosterone-salt (1 µg.h(-1)), with or without administration of either red wine polyphenols, Provinols™ (20 mg.kg(-1).day(-1)), or spironolactone (30 mg.kg(-1).day(-1)) for 4 weeks. Microparticles, arterial stiffness, nitric oxide (NO) spin trapping, and mesenteric arterial function were measured. Aldosterone-salt rats showed increased microparticle levels, including those originating from platelets, endothelium and erythrocytes. Hypertension resulted in enhanced aortic stiffness accompanied by increased circulating and aortic NO levels and an upregulation of aortic inducible NO-synthase, NFκB, superoxide anions and nitrotyrosine. Flow-induced dilatation was reduced in mesenteric arteries. These effects were prevented by spironolactone. Provinols™ did not reduce arterial stiffness or systolic hypertension but had effects similar to those of spironolactone on endothelial function assessed by flow-mediated vasodilatation, microparticle generation, aortic NO levels and oxidative stress and apoptosis in the vessel wall. Neither the contractile response nor endothelium-dependent relaxation in mesenteric arteries differed between groups. The in vivo effects of Provinols™ were not mediated by mineralocorticoid receptors or changes in shear stress. In conclusion, vascular remodelling and endothelial dysfunction in aldosterone-salt-mediated hypertension are associated with increased circulating microparticles. Polyphenols prevent the enhanced release of microparticles, macrovascular inflammation and oxidative stress, and microvascular endothelial dysfunction independently of blood pressure, shear stress and mineralocorticoid receptor activation in a model of hyperaldosteronism. | | | 22808030
 |
Local oxidative stress expansion through endothelial cells--a key role for gap junction intercellular communication.
Feine, I; Pinkas, I; Salomon, Y; Scherz, A
PloS one
7
e41633
2012
Show Abstract
Major circulation pathologies are initiated by oxidative insult expansion from a few injured endothelial cells to distal sites; this possibly involves mechanisms that are important to understanding circulation physiology and designing therapeutic management of myocardial pathologies. We tested the hypothesis that a localized oxidative insult of endothelial cells (ECs) propagates through gap junction inter-cellular communication (GJIC).Cultures comprising the bEnd.3 cell line, that have been established and recognized as suitable for examining communication among ECs, were used to study the propagation of a localized oxidative insult to remote cells. Spatially confined near infrared illumination of parental or genetically modified bEnd.3 cultures, pretreated with the photosensitizer WST11, generated O(2)•(-) and •OH radicals in the illuminated cells. Time-lapse fluorescence microscopy, utilizing various markers, and other methods, were used to monitor the response of non-illuminated bystander and remote cells. Functional GJIC among ECs was shown to be mandatory for oxidative insult propagation, comprising de-novo generation of reactive oxygen and nitrogen species (ROS and RNS, respectively), activation and nuclear translocation of c-Jun N-terminal kinase, followed by massive apoptosis in all bystander cells adjacent to the primarily injured ECs. The oxidative insult propagated through GJIC for many hours, over hundreds of microns from the primary photogeneration site. This wave is shown to be limited by intracellular ROS scavenging, chemical GJIC inhibition or genetic manipulation of connexin 43 (a key component of GJIC).Localized oxidative insults propagate through GJIC between ECs, while stimulating de-novo generation of ROS and RNS in bystander cells, thereby driving the insult's expansion. | | | 22911831
 |
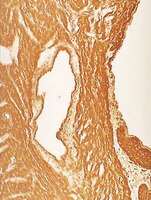
Role of nitric oxide synthases in elastase-induced emphysema.
Boyer, L; Plantier, L; Dagouassat, M; Lanone, S; Goven, D; Caramelle, P; Berrehar, F; Kerbrat, S; Dinh-Xuan, AT; Crestani, B; Le Gouvello, S; Boczkowski, J
Laboratory investigation; a journal of technical methods and pathology
91
353-62
2011
Show Abstract
Nitric oxide (NO) in combination with superoxide produces peroxynitrites and induces protein nitration, which participates in a number of chronic degenerative diseases. NO is produced at high levels in the human emphysematous lung, but its role in this disease is unknown. The aim of this study was to determine whether the NO synthases contribute to the development of elastase-induced emphysema in mice. nNOS, iNOS, and eNOS were quantified and immunolocalized in the lung after a tracheal instillation of elastase in mice. To determine whether eNOS or iNOS had a role in the development of emphysema, mice bearing a germline deletion of the eNOS and iNOS genes and mice treated with a pharmacological iNOS inhibitor were exposed to elastase. Protein nitration was determined by immunofluorescence, protein oxidation was determined by ELISA. Inflammation and MMP activity were quantified by cell counts, RT-PCR and zymography in bronchoalveolar lavage fluid. Cell proliferation was determined by Ki67 immunostaining. Emphysema was quantified morphometrically. iNOS and eNOS were diffusely upregulated in the lung of elastase-treated mice and a 12-fold increase in the number of 3-nitrotyrosine-expressing cells was observed. Over 80% of these cells were alveolar type 2 cells. In elastase-instilled mice, iNOS inactivation reduced protein nitration and increased protein oxidation but had no effect on inflammation, MMP activity, cell proliferation or the subsequent development of emphysema. eNOS inactivation had no effect. In conclusion, in the elastase-injured lung, iNOS mediates protein nitration in alveolar type 2 cells and alleviates oxidative injury. Neither eNOS nor iNOS are required for the development of elastase-induced emphysema. | | | 20956973
 |
Microparticles from apoptotic monocytes enhance nitrosative stress in human endothelial cells.
Mastronardi, Maria Letizia, et al.
Fundam Clin Pharmacol, 25: 653-60 (2011)
2011
Show Abstract
Microparticles are membrane vesicles with procoagulant and proinflammatory properties released during cell activation or apoptosis. Microparticles from monocytes have been implicated in atherosclerosis and vascular inflammation, but their direct effects on endothelial cells are not completely elucidated. The present study was designed to dissect the signaling pathways of monocytic microparticles in endothelial cells with respect to both NO pathway and reactive oxygen species. Microparticles were produced by treatment of human monocytic cell line THP-1 with the apoptotic agent VP-16. Human endothelial cells were treated with monocytic microparticles and then, we studied their effects on nitrosative and oxidative stresses. Incubation of human endothelial cells with microparticles enhanced the production of NO without affecting superoxide anions generation. Microparticles did not affect endothelial NO synthase expression and its phosphorylation. Interestingly, microparticles decreased caveolin-1 expression and increased its phosphorylation. Inhibition of PI-3-kinase or MEK1/2 reversed the effects of microparticles on caveolin-1 expression but not its phosphorylation. Moreover, microparticles increased nitration of several proteins, reflecting peroxynitrite production, which was prevented by blockade of PI-3-kinase pathway. In summary, monocyte microparticles active multiple pathways related to nitrosative stress in endothelial cells including both PI-3-kinase and ERK1/2 in the regulation of caveolin-1 expression. These data underscore the pleiotropic effect of microparticles on endothelial cells and suggest that they probably play a critical role on vascular function. | | | 21105910
 |
Relaxin ameliorates hypertension and increases nitric oxide metabolite excretion in angiotensin II but not N(ω)-nitro-L-arginine methyl ester hypertensive rats.
Sasser, JM; Molnar, M; Baylis, C
Hypertension
58
197-204
2011
Show Abstract
Previous findings suggest a potential therapeutic action of relaxin, the putative vasodilatory signal of normal pregnancy, in some forms of cardiovascular disease. However, the mechanisms underlying the beneficial effects of relaxin have not been fully elucidated. The purpose of this study was to determine whether the vasodilatory effects of relaxin are dependent on activation of NO synthase. We examined the effect of relaxin in male Sprague-Dawley rats given angiotensin II (Ang II; 200 ng/kg per minute SC by minipump), the NO synthase inhibitor N(ω)-nitro-l-arginine methyl ester (l-NAME; 1.5 mg/100 g IV followed by 150 mg/L in drinking water), or vehicle for 3 weeks. After 7 days of Ang II or l-NAME, mean arterial pressure was elevated compared with baseline. Relaxin was administered (4 μg/h, SC by minipump) for the next 2 weeks of Ang II, l-NAME, or vehicle treatment. Two-week relaxin treatment alone slightly reduced mean arterial pressure in normotensive rats. Three weeks of either Ang II or l-NAME treatment alone produced hypertension, albuminuria, mild glomerular sclerosis, reduced nitric oxide metabolite excretion, and increased oxidative stress (excretion of hydrogen peroxide and thiobarbituric acid reactive substances and renal cortex nitrotyrosine abundance). Relaxin reduced mean arterial pressure, albumin excretion, and oxidative stress markers and preserved glomerular structure and nitric oxide metabolite excretion in Ang II-treated rats; however, relaxin did not attenuate these changes in the rats treated with l-NAME. None of the treatments affected protein abundance of neuronal or endothelial NO synthase in the kidney cortex. These data suggest that the vasodilatory effects of relaxin are dependent on a functional NO synthase system and increased NO bioavailability possibly because of a reduction in oxidative stress. | Western Blotting | | 21670419
 |
Butyrylcholinesterase inhibitors ameliorate cognitive dysfunction induced by amyloid-β peptide in mice.
Yoko Furukawa-Hibi,Tursun Alkam,Atsumi Nitta,Akihiro Matsuyama,Hiroyuki Mizoguchi,Kazuhiko Suzuki,Saliha Moussaoui,Qian-Sheng Yu,Nigel H Greig,Taku Nagai,Kiyofumi Yamada
Behavioural brain research
225
2011
Show Abstract
The cholinesterase inhibitor, rivastigmine, ameliorates cognitive dysfunction and is approved for the treatment of Alzheimer's disease (AD). Rivastigmine is a dual inhibitor of acetylcholinesterase (AChE) and butyrylcholinesterase (BuChE); however, the impact of BuChE inhibition on cognitive dysfunction remains to be determined. We compared the effects of a selective BuChE inhibitor, N1-phenethyl-norcymserine (PEC), rivastigmine and donepezil (an AChE-selective inhibitor) on cognitive dysfunction induced by amyloid-β peptide (Aβ(1-40)) in mice. Five-week-old imprinting control region (ICR) mice were injected intracerebroventricularly (i.c.v.) with either Aβ(1-40) or the control peptide Aβ(40-1) on Day 0, and their recognition memory was analyzed by a novel object recognition test. Treatment with donepezil (1.0mg/kg), rivastigmine (0.03, 0.1, 0.3mg/kg) or PEC (1.0, 3.0mg/kg) 20min prior to, or immediately after the acquisition session (Day 4) ameliorated the Aβ(1-40) induced memory impairment, indicating a beneficial effect on memory acquisition and consolidation. In contrast, none of the investigated drugs proved effective when administrated before the retention session (Day 5). Repeated daily administration of donepezil, rivastigmine or PEC, on Days 0-3 inclusively, ameliorated the cognitive dysfunction in Aβ(1-40) challenged mice. Consistent with the reversal of memory impairments, donepezil, rivastigmine or PEC treatment significantly reduced Aβ(1-40) induced tyrosine nitration of hippocampal proteins, a marker of oxidative damage. These results indicate that BuChE inhibition, as well as AChE inhibition, is a viable therapeutic strategy for cognitive dysfunction in AD. | | | 21820013
 |