Extracellular matrix effect on RhoA signaling modulation in vascular smooth muscle cells.
Soon-Mi Lim,Bryan A Kreipe,Jerome Trzeciakowski,Larry Dangott,Andreea Trache
Experimental cell research
316
2010
Show Abstract
Morphological adaptations of vascular smooth muscle cells (VSMC) to the mechanically active environment in which they reside, are mediated by direct interactions with the extracellular matrix (ECM) which induces physiological changes at the intracellular level. This study aimed to analyze the effects of the ECM on RhoA-induced mechanical signaling that controls actin organization and focal adhesion formation. VSMC were transfected with RhoA constructs (wild type, dominant negative or constitutively active) and plated on different ECM proteins used as substrate (fibronectin, collagen IV, collagen I, and laminin) or poly-l-lysine as control. Morphological changes of the VSMC were detected by fluorescence confocal microscopy and total internal reflection fluorescence (TIRF) microscopy, and were independently verified using adhesion assays and Western blot analysis. Our results showed that the ECM has an important role in cell spreading, adhesion and morphology with a direct effect on modulating RhoA signaling. RhoA activity significantly affected the stress fibers and focal adhesions reorganization, but in a context imposed by the ECM. Thus, RhoA activity modulation in VSMC induced an increased activation of stress fibers and FA formation at 5h, while a significant inhibition was recorded at 24h after plating on the different ECM. Our findings provide biophysical evidence that ECM modulates VSMC response to mechanical stimuli inducing intracellular biochemical signaling involved in cellular adaptation to the local microenvironment. | | 20599954
 |
Rescue of migratory defects of Ehlers-Danlos syndrome fibroblasts in vitro by type V collagen but not insulin-like binding protein-1.
Viglio, Simona, et al.
J. Invest. Dermatol., 128: 1915-9 (2008)
2008
| Human | 18305566
 |
Phagocytosis and remodeling of collagen matrices.
Leah C Abraham,J Fred Dice,Kyongbum Lee,David L Kaplan
Experimental cell research
313
2007
Show Abstract
The biodegradation of collagen and the deposition of new collagen-based extracellular matrices are of central importance in tissue remodeling and function. Similarly, for collagen-based biomaterials used in tissue engineering, the degradation of collagen scaffolds with accompanying cellular infiltration and generation of new extracellular matrix is critical for the integration of in vitro grown tissues in vivo. In earlier studies we observed significant impact of collagen structure on primary lung fibroblast behavior in vitro in terms of collagen uptake and matrix remodeling. Therefore, in the present work, the response of human fibroblasts (IMR-90) to the structural state of collagen was studied with respect to phagocytosis in the presence and absence of inhibitors. Protein content and transcript levels for collagen I (Col-1), matrix metalloproteinase 1 (MMP-1), matrix metalloproteinase 2 (MMP-2), tissue inhibitor of matrix metalloproteinase 1 (TIMP-1), tissue inhibitor of matrix metalloproteinase 2 (TIMP-2), and heat shock protein 70 (HSP-70) were characterized as a function of collagen matrix concentration, structure and cell culture time to assess effects on cellular collagen matrix remodeling processes. Phagocytosis of collagen was assessed quantitatively by the uptake of collagen-coated fluorescent beads incorporated into the collagen matrices. Significantly higher levels of collagen phagocytosis were observed for the cells grown on the denatured collagen versus native collagen matrices. Significant reduction in collagen phagocytosis was observed by blocking several phagocytosis pathways when the cells were grown on denatured collagen versus non-denatured collagen. Collagen phagocytosis inhibition effects were significantly greater for PDL57 IMR-90 cells versus PDL48 cells, reflecting a reduced number of collagen processing pathways available to the older cells. Transcript levels related to the deposition of new extracellular matrix proteins varied as a function of the structure of the collagen matrix presented to the cells. A four-fold increase in transcript level of Col-1 and a higher level of collagen matrix incorporation were observed for cells grown on denatured collagen versus cells grown on non-denatured collagen. The data suggest that biomaterial matrices incorporating denatured collagen may promote more active remodeling toward new extracellular matrices in comparison to cells grown on non-denatured collagen. A similar effect of cellular action toward denatured (wound-related) collagen in the remodeling of tissues in vivo may have significant impact on tissue regeneration as well as the progression of collagen-related diseases. Full Text Article | | 17276428
 |
Matrix metalloproteinase 1 interacts with neuronal integrins and stimulates dephosphorylation of Akt.
Conant, K; St Hillaire, C; Nagase, H; Visse, R; Gary, D; Haughey, N; Anderson, C; Turchan, J; Nath, A
The Journal of biological chemistry
279
8056-62
2004
Show Abstract
Several studies have demonstrated that matrix metalloproteinases (MMPs) are cytotoxic. The responsible mechanisms, however, are not well understood. MMPs may promote cytotoxicity through their ability to disrupt or degrade matrix proteins that support cell survival, and MMPs may also cleave substrates to generate molecules that stimulate cell death. In addition, MMPs may themselves act on cell surface receptors that affect cell survival. Among such receptors is the alpha(2)beta(1) integrin, a complex that has previously been linked to leukocyte death. In the present study we show that human neurons express alpha(2)beta(1) and that pro-MMP-1 interacts with this integrin complex. We also show that stimulation of neuronal cultures with MMP-1 is associated with a rapid reduction in the phosphorylation of Akt, a kinase that can influence caspase activity and cell survival. Moreover, MMP-1-associated dephosphorylation of Akt is inhibited by a blocking antibody to the alpha(2) integrin, but not by batimastat, an inhibitor of MMP-1 enzymatic activity. Such dephosphorylation is also stimulated by a catalytic mutant of pro-MMP-1. Additional studies show that MMP-1 causes neuronal death, which is significantly diminished by both a general caspase inhibitor and anti-alpha(2) but not by batimastat. Together, these results suggest that MMP-1 can stimulate dephosphorylation of Akt and neuronal death through a non-proteolytic mechanism that involves changes in integrin signaling. | | 14679206
 |
Molecular pathway for cancer metastasis to bone
De, Sarmishtha, et al
J Biol Chem, 278:39044-50 (2003)
2003
| | 12885781
 |
Platelet alpha2beta1 integrin activation: contribution of ligand internalization and the alpha2-cytoplasmic domain.
Wang, Zhengyan, et al.
Blood, 102: 1307-15 (2003)
2003
Show Abstract
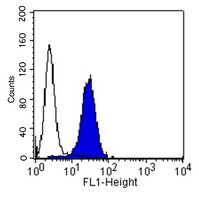
The alpha2beta1 integrin is a major collagen receptor on platelets. Although it has been proposed that alpha2beta1, like alphaIIbbeta3, undergoes agonist-induced activation, neither the potential contributions of alpha2beta1 receptor/ligand internalization to the increase in ligand binding nor the roles of the alpha2 and beta1 cytoplasmic domains in activation of this integrin have been previously explored. Activation of alpha2beta1 was assessed with fluorescein isothiocyanate-labeled soluble type I collagen binding to platelets by flow cytometry. Although collagen internalization in response to agonist activation of platelets was significant, agonist-induced collagen binding still occurred under conditions that block internalization, with minimal changes in cell surface alpha2beta1 expression. Introduction of cell-permeable peptides containing the alpha2 cytoplasmic tail, and especially the membrane proximal KLGFFKR domain, induced alpha2beta1 activation in resting platelets, whereas a cell-permeable peptide containing the beta1 cytoplasmic tail was without effect. Thus, collagen binding to stimulated platelets is increased due to alpha2beta1 activation, in addition to internalization, and the GFFKR motif appears to play an important role in the activation process. | | 12738679
 |
The thrombospondin receptor CD47 (IAP) modulates and associates with alpha2 beta1 integrin in vascular smooth muscle cells.
Wang, X Q and Frazier, W A
Mol. Biol. Cell, 9: 865-74 (1998)
1998
Show Abstract
The carboxyl-terminal domain of thrombospondin-1 enhances the migration and proliferation of smooth muscle cells. Integrin-associated protein (IAP or CD47) is a receptor for the thrombospondin-1 carboxyl-terminal cell-binding domain and binds the agonist peptide 4N1K (kRFYVVMWKk) from this domain. 4N1K peptide stimulates chemotaxis of both human and rat aortic smooth muscle cells on gelatin-coated filters. The migration on gelatin is specifically blocked by monoclonal antibodies against IAP and a beta1 integrin, rather than alphav beta3 as found previously for 4N1K-stimulated chemotaxis of endothelial cells on gelatin. Both human and rat smooth muscle cells displayed a weak migratory response to soluble type I collagen; however, the presence of 4N1K peptide or intact thrombospondin-1 provoked a synergistic chemotactic response that was partially blocked by antibodies to alpha2 and beta1 integrin subunits and to IAP. A combination of antialpha2 and IAP monoclonal antibodies completely blocked chemotaxis. RGD peptide and antialphav beta3 mAb were without effect. 4N1K and thrombospondin-1 did not augment the chemotactic response of smooth muscle cells to fibronectin, vitronectin, or collagenase-digested type I collagen. Complex formation between alpha2 beta1 and IAP was detected by the coimmunoprecipitation of both alpha2 and beta1 integrin subunits with IAP. These data suggest that IAP can associate with alpha2 beta1 integrin and modulate its function. | | 9529384
 |
Fibroblast growth factor-2 potentiates vascular smooth muscle cell migration to platelet-derived growth factor: upregulation of alpha2beta1 integrin and disassembly of actin filaments
Pickering, J G, et al
Circ Res, 80:627-37 (1997)
1997
| | 9130443
 |
Integrin VLA-2 (alpha2beta1) function in postextravasation movement of human rhabdomyosarcoma RD cells in the liver
Hangan, D, et al
Cancer Res, 56:3142-9 (1996)
1996
| | 8674074
 |