Intranasal immunization with W 80 5EC adjuvanted recombinant RSV rF-ptn enhances clearance of respiratory syncytial virus in a mouse model.
Passmore, C; Makidon, PE; O'Konek, JJ; Zahn, JA; Pannu, J; Hamouda, T; Bitko, V; Myc, A; Lukacs, NW; Fattom, A; Baker, JR
Human vaccines & immunotherapeutics
10
615-22
2014
요약 표시
Respiratory Syncytial Virus (RSV) is a ubiquitous virus that infects almost all people by age two and is a major source of respiratory illness in infants, the elderly and others with compromised immune systems. Currently there is no available vaccine. Prior efforts using formalin-inactivated RSV (FI-RSV) were associated with enhanced respiratory disease upon viral exposure following clinical vaccine trials. Several researchers and pharmaceutical companies have utilized vector-associated live attenuated RSV vaccines in pre-clinical and clinical studies. Another attractive approach, however, is a subunit vaccine which would be easier to produce and quality control. Our group has previously demonstrated in a murine model of infection that intranasal immunization with nanoemulsion-inactivated and adjuvanted RSV induces humoral and cellular immune responses, resulting in protection against RSV infection. The present studies characterize the immune responses elicited by intranasal RSV F protein adjuvanted with nanoemulsion. Intranasal application of nanoemulsion adjuvanted F protein induced a rapid and robust systemic and mucosal antibody response, as well as protection against subsequent RSV challenge. Importantly, RSV challenge in immunized animals did not elicit airway hyper-reactivity, a Th2-skewed immune response or immunopathology associated with hypersensitivity reactions with formalin-inactivated vaccine. These results suggest that RSV F protein adjuvanted with nanoemulsion may be a good mucosal vaccine candidate. Formulating RSV F protein in nanoemulsion creates a well-defined and well-controlled vaccine that can be delivered intranasally to induce T cell mediated immunity without inducing enhanced disease associated with the mouse model of FI-RSV vaccination and infection. | 24326268
 |
Respiratory syncytial virus (RSV) infection in elderly mice results in altered antiviral gene expression and enhanced pathology.
Wong, TM; Boyapalle, S; Sampayo, V; Nguyen, HD; Bedi, R; Kamath, SG; Moore, ML; Mohapatra, S; Mohapatra, SS
PloS one
9
e88764
2014
요약 표시
Elderly persons are more susceptible to RSV-induced pneumonia than young people, but the molecular mechanism underlying this susceptibility is not well understood. In this study, we used an aged mouse model of RSV-induced pneumonia to examine how aging alters the lung pathology, modulates antiviral gene expressions, and the production of inflammatory cytokines in response to RSV infection. Young (2-3 months) and aged (19-21 months) mice were intranasally infected with mucogenic or non-mucogenic RSV strains, lung histology was examined, and gene expression was analyzed. Upon infection with mucogenic strains of RSV, leukocyte infiltration in the airways was elevated and prolonged in aged mice compared to young mice. Minitab factorial analysis identified several antiviral genes that are influenced by age, infection, and a combination of both factors. The expression of five antiviral genes, including pro-inflammatory cytokines IL-1β and osteopontin (OPN), was altered by both age and infection, while age was associated with the expression of 15 antiviral genes. Both kinetics and magnitude of antiviral gene expression were diminished as a result of older age. In addition to delays in cytokine signaling and pattern recognition receptor induction, we found TLR7/8 signaling to be impaired in alveolar macrophages in aged mice. In vivo, induction of IL-1β and OPN were delayed but prolonged in aged mice upon RSV infection compared to young. In conclusion, this study demonstrates inherent differences in response to RSV infection in young vs. aged mice, accompanied by delayed antiviral gene induction and cytokine signaling. | 24558422
 |
Protection and mechanism of action of a novel human respiratory syncytial virus vaccine candidate based on the extracellular domain of small hydrophobic protein.
Schepens, B; Sedeyn, K; Vande Ginste, L; De Baets, S; Schotsaert, M; Roose, K; Houspie, L; Van Ranst, M; Gilbert, B; van Rooijen, N; Fiers, W; Piedra, P; Saelens, X
EMBO molecular medicine
6
1436-54
2014
요약 표시
Infections with human respiratory syncytial virus (HRSV) occur globally in all age groups and can have devastating consequences in young infants. We demonstrate that a vaccine based on the extracellular domain (SHe) of the small hydrophobic (SH) protein of HRSV, reduced viral replication in challenged laboratory mice and in cotton rats. We show that this suppression of viral replication can be transferred by serum and depends on a functional IgG receptor compartment with a major contribution of FcγRI and FcγRIII. Using a conditional cell depletion method, we provide evidence that alveolar macrophages are involved in the protection by SHe-specific antibodies. HRSV-infected cells abundantly express SH on the cell surface and are likely the prime target of the humoral immune response elicited by SHe-based vaccination. Finally, natural infection of humans and experimental infection of mice or cotton rats does not induce a strong immune response against HRSV SHe. Using SHe as a vaccine antigen induces immune protection against HRSV by a mechanism that differs from the natural immune response and from other HRSV vaccination strategies explored to date. Hence, HRSV vaccine candidates that aim at inducing protective neutralizing antibodies or T-cell responses could be complemented with a SHe-based antigen to further improve immune protection. | 25298406
 |
Host cell entry of respiratory syncytial virus involves macropinocytosis followed by proteolytic activation of the F protein.
Krzyzaniak, MA; Zumstein, MT; Gerez, JA; Picotti, P; Helenius, A
PLoS pathogens
9
e1003309
2013
요약 표시
Respiratory Syncytial Virus (RSV) is a highly pathogenic member of the Paramyxoviridae that causes severe respiratory tract infections. Reports in the literature have indicated that to infect cells the incoming viruses either fuse their envelope directly with the plasma membrane or exploit clathrin-mediated endocytosis. To study the entry process in human tissue culture cells (HeLa, A549), we used fluorescence microscopy and developed quantitative, FACS-based assays to follow virus binding to cells, endocytosis, intracellular trafficking, membrane fusion, and infection. A variety of perturbants were employed to characterize the cellular processes involved. We found that immediately after binding to cells RSV activated a signaling cascade involving the EGF receptor, Cdc42, PAK1, and downstream effectors. This led to a series of dramatic actin rearrangements; the cells rounded up, plasma membrane blebs were formed, and there was a significant increase in fluid uptake. If these effects were inhibited using compounds targeting Na⁺/H⁺ exchangers, myosin II, PAK1, and other factors, no infection was observed. The RSV was rapidly and efficiently internalized by an actin-dependent process that had all hallmarks of macropinocytosis. Rather than fusing with the plasma membrane, the viruses thus entered Rab5-positive, fluid-filled macropinosomes, and fused with the membranes of these on the average 50 min after internalization. Rab5 was required for infection. To find an explanation for the endocytosis requirement, which is unusual among paramyxoviruses, we analyzed the fusion protein, F, and could show that, although already cleaved by a furin family protease once, it underwent a second, critical proteolytic cleavage after internalization. This cleavage by a furin-like protease removed a small peptide from the F1 subunits, and made the virus infectious. | 23593008
 |
Recombinant influenza virus carrying the respiratory syncytial virus (RSV) F85-93 CTL epitope reduces RSV replication in mice.
De Baets, S; Schepens, B; Sedeyn, K; Schotsaert, M; Roose, K; Bogaert, P; Fiers, W; Saelens, X
Journal of virology
87
3314-23
2013
요약 표시
Respiratory syncytial virus (RSV) is the leading cause of lower respiratory tract infections in infants worldwide. Despite decades of research, there is still no registered vaccine available for this major pathogen. We investigated the protective efficacy of a recombinant influenza virus, PR8/NA-F(85-93), that carries the RSV CD8(+) T cell epitope F(85-93) in its neuraminidase stalk. F(85-93)-specific cytotoxic T lymphocytes (CTLs) were induced in mice after a single intranasal immunization with PR8/NA-F(85-93) virus, and these CTLs provided a significant reduction in the lung viral load upon a subsequent challenge with RSV. To avoid influenza-induced morbidity, we treated mice with matrix protein 2 (M2e)-specific monoclonal antibodies before PR8/NA-F(85-93) virus infection. Treatment with anti-M2e antibodies reduced the infiltration of immune cells in the lungs upon PR8/NA-F(85-93) infection, whereas the formation of inducible bronchus-associated lymphoid tissue was not affected. Moreover, this treatment prevented body weight loss yet still permitted the induction of RSV F-specific T cell responses and significantly reduced RSV replication upon challenge. These results demonstrate that it is possible to take advantage of the infection-permissive protection of M2e-specific antibodies against influenza A virus to induce heterologous CD8(+) T cell-mediated immunity by an influenza A virus vector expressing the RSV F(85-93) epitope. | 23302879
 |
Respiratory syncytial virus (RSV) suppression of glucocorticoid receptor phosphorylation does not account for repression of transactivation.
Webster Marketon, JI; Corry, J
FEBS open bio
3
305-9
2013
요약 표시
Respiratory syncytial virus (RSV)-induced bronchiolitis in infants, although inflammatory in nature, is not responsive to glucocorticoids. We have recently shown that RSV-infected lung epithelial cells have impaired glucocorticoid receptor (GR)-mediated transactivation. In this study, we show that the N-terminal region of GR is required for RSV repression of GR transactivation and that RSV infection of lung epithelial cells reduces ligand-dependent GR phosphorylation at serine 211 and serine 226. However, we also show that these changes in GR phosphorylation do not account for the RSV repression of GR transactivation suggesting other regions of the GR N-terminus must also be involved. | 23951552
 |
Nanobodies® specific for respiratory syncytial virus fusion protein protect against infection by inhibition of fusion.
Schepens, B; Ibañez, LI; De Baets, S; Hultberg, A; Bogaert, P; De Bleser, P; Vervalle, F; Verrips, T; Melero, J; Vandevelde, W; Vanlandschoot, P; Saelens, X
The Journal of infectious diseases
204
1692-701
2011
요약 표시
Despite the medical importance of respiratory syncytial virus (RSV) infections, there is no vaccine or therapeutic agent available. Prophylactic administration of palivizumab, a humanized monoclonal RSV fusion (F) protein-specific antibody, can protect high-risk children. Previously, we have demonstrated that RSV can be neutralized by picomolar concentrations of a camelid immunoglobulin single-variable domain that binds the RSV protein F (F-VHHb nanobodies). Here, we investigated the mechanism by which these nanobodies neutralize RSV and tested their antiviral activity in vivo. We demonstrate that bivalent RSV F-specific nanobodies neutralize RSV infection by inhibiting fusion without affecting viral attachment. The ability of RSV F-specific nanobodies to protect against RSV infection was investigated in vivo. Intranasal administration of bivalent RSV F-specific nanobodies protected BALB/c mice from RSV infection, and associated pulmonary inflammation. Moreover, therapeutic treatment with these nanobodies after RSV infection could reduce viral replication and reduced pulmonary inflammation. Thus, nanobodies are promising therapeutic molecules for treatment of RSV. | 21998474
 |
Respiratory syncytial virus represses glucocorticoid receptor-mediated gene activation.
Hinzey, A; Alexander, J; Corry, J; Adams, KM; Claggett, AM; Traylor, ZP; Davis, IC; Webster Marketon, JI
Endocrinology
152
483-94
2011
요약 표시
Respiratory syncytial virus (RSV) is a common cause of bronchiolitis in infants. Although antiinflammatory in nature, glucocorticoids have been shown to be ineffective in the treatment of RSV-induced bronchiolitis and wheezing. In addition, the effectiveness of glucocorticoids at inhibiting RSV-induced proinflammatory cytokine production in cell culture has been questioned. In this study, we have investigated the effect of RSV infection on glucocorticoid-induced gene activation in lung epithelium-derived cells. We show that RSV infection inhibits dexamethasone induction of three glucocorticoid receptor (GR)-regulated genes (glucocorticoid-inducible leucine zipper, FK506 binding protein, and MAPK phosphatase 1) in A549, BEAS-2B cells, and primary small airway epithelial cells. UV irradiation of the virus prevents this repression, suggesting that viral replication is required. RSV is known to activate the nuclear factor κB (NFκB) pathway, which is mutually antagonistic towards the GR pathway. However, specific inhibition of NFκB had no effect on the repression of GR-induced genes by RSV infection, indicating that RSV repression of GR is independent of NFκB. RSV infection of A549 cells does not alter GR protein levels or GR nuclear translocation but does reduce GR binding to the promoters of the glucocorticoid responsive genes analyzed in this study. Repression of GR by RSV infection may account for the apparent clinical ineffectiveness of glucocorticoids in RSV bronchiolitis therapy. In addition, this data adds to our previously published data suggesting that GR may be a general target for infectious agents. Identifying the mechanisms through which this suppression occurs may lead to the development of novel therapeutics. 기사 전문 | 21190962
 |
Differential pathogenesis of respiratory syncytial virus clinical isolates in BALB/c mice.
Stokes, KL; Chi, MH; Sakamoto, K; Newcomb, DC; Currier, MG; Huckabee, MM; Lee, S; Goleniewska, K; Pretto, C; Williams, JV; Hotard, A; Sherrill, TP; Peebles, RS; Moore, ML
Journal of virology
85
5782-93
2011
요약 표시
Airway mucus is a hallmark of respiratory syncytial virus (RSV) lower respiratory tract illness. Laboratory RSV strains differentially induce airway mucus production in mice. Here, we tested the hypothesis that RSV strains differ in pathogenesis by screening six low-passage RSV clinical isolates for mucogenicity and virulence in BALB/cJ mice. The RSV clinical isolates induced variable disease severity, lung interleukin-13 (IL-13) levels, and gob-5 levels in BALB/cJ mice. We chose two of these clinical isolates for further study. Infection of BALB/cJ mice with RSV A2001/2-20 (2-20) resulted in greater disease severity, higher lung IL-13 levels, and higher lung gob-5 levels than infection with RSV strains A2, line 19, Long, and A2001/3-12 (3-12). Like the line 19 RSV strain, the 2-20 clinical isolate induced airway mucin expression in BALB/cJ mice. The 2-20 and 3-12 RSV clinical isolates had higher lung viral loads than laboratory RSV strains at 1 day postinfection (p.i.). This increased viral load correlated with higher viral antigen levels in the bronchiolar epithelium and greater histopathologic changes at 1 day p.i. The A2 RSV strain had the highest peak viral load at day 4 p.i. RSV 2-20 infection caused epithelial desquamation, bronchiolitis, airway hyperresponsiveness, and increased breathing effort in BALB/cJ mice. We found that RSV clinical isolates induce variable pathogenesis in mice, and we established a mouse model of clinical isolate strain-dependent RSV pathogenesis that recapitulates key features of RSV disease. | 21471228
 |
Recombinant simian varicella viruses expressing respiratory syncytial virus antigens are immunogenic.
Ward, TM; Traina-Dorge, V; Davis, KA; Gray, WL
The Journal of general virology
89
741-50
2008
요약 표시
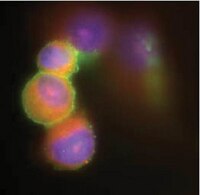
Recombinant simian varicella viruses (rSVVs) were engineered to express respiratory syncytial virus (RSV) antigens. The RSV surface glycoprotein G and second matrix protein M2 (22k) genes were cloned into the SVV genome, and recombinant viruses were characterized in vitro and in vivo. rSVVs were also engineered to express the membrane-anchored or secreted forms of the RSV-G protein as well as an RSV G lacking its chemokine mimicry motif (CX3C), which may have different effects on priming the host immune response. The RSV genes were efficiently expressed in rSVV/RSV-infected Vero cells as RSV-G and -M2 transcripts were detected by RT-PCR, and RSV antigens were detected by immunofluorescence and immunoblot assays. The rSVVs replicated efficiently in Vero cell culture. Rhesus macaques immunized with rSVV/RSV-G and rSVV/RSV-M2 vaccines produced antibody responses to SVV and RSV antigens. The results demonstrate that recombinant varicella viruses are suitable vectors for the expression of RSV antigens and may represent a novel vaccine strategy for immunization against both pathogens. | 18272766
 |