Upregulation of SOCS-1 by Nutlin-3 in acute myeloid leukemia cells but not in primary normal cells.
Tisato, V; Norcio, A; Celeghini, C; Milani, D; Gonelli, A; Secchiero, P
Clinics (São Paulo, Brazil)
69
68-74
2014
概要を表示する
It has been shown that SOCS-1 plays an important role in the proper control of cytokine/growth factor responses and acts as a tumor suppressor in acute myeloid leukemias. Therefore, the objective of the present study was to evaluate the in vitro effect of treatment with Nutlin-3, a small molecule inhibitor of the MDM2/p53 interaction, on the expression of the suppressor of cytokine signaling 1 in primary acute myeloid leukemia cells and in myeloid cell lines with differential p53 status.The expression of the suppressor of cytokine signaling 1 was quantitatively analyzed by real-time PCR in myeloid p53wild-type (OCI and MOLM) and p53null HL-60, leukemic cell lines, in patient-derived acute myeloid leukemia blasts, and in primary normal cell types, such as macrophages, endothelial cells, and bone marrow mesenchymal stem cells. The p53-dependence of the suppressor of cytokine signaling 1 upregulation that is induced by Nutlin-3 was analyzed in experiments performed using siRNA for p53, while the functional upregulation of the suppressor of cytokine signaling 1 was analyzed by assessing the levels of phosphorylated STAT-3.Nutlin-3 significantly upregulated the transcription of the suppressor of cytokine signaling 1 in p53wild-type OCI and MOLM but not in p53deleted p53null HL60, myeloid leukemic cell lines, as well as in primary acute myeloid leukemia blasts. Conversely, and somewhat unexpectedly, Nutlin-3 did not modulate the suppressor of cytokine signaling 1 expression in primary normal macrophages, endothelial cells, and bone marrow mesenchymal stem cells. The p53-dependent upregulation of the suppressor of cytokine signaling 1 by Nutlin-3 was associated with the downregulation of phosphorylated STAT-3, a major molecular target of the suppressor of cytokine signaling 1.Overall, our data suggest a potential role for the suppressor of cytokine signaling 1 as a therapeutic target of Nutlin-3 in p53 wild-type acute myeloid leukemias. | 24473562
 |
EMP1, a novel poor prognostic factor in pediatric leukemia regulates prednisolone resistance, cell proliferation, migration and adhesion.
Ariës, IM; Jerchel, IS; van den Dungen, RE; van den Berk, LC; Boer, JM; Horstmann, MA; Escherich, G; Pieters, R; den Boer, ML
Leukemia
2014
概要を表示する
Still 20% of pediatric acute lymphoblastic leukemia (ALL) patients relapse on or after current treatment strategies. Treatment failure is associated with resistance to prednisolone. We aimed to find new druggable targets that modulate prednisolone resistance. We generated microarray gene expression profiles of 256 pediatric ALL patient samples and identified a 3.4-fold increase in epithelial membrane protein 1 (EMP1) expression in in vitro prednisolone-resistant compared with -sensitive patients (P=0.003). EMP1 silencing in six precursor-B ALL (BCP-ALL) and T-ALL cell lines induced apoptosis and cell-cycle arrest leading to 84.1±4.5% reduction in survival compared with non-silencing control transduced cells (non-silencing control short hairpin, shNSC) (P=0.014). Moreover, EMP1 silencing sensitized to prednisolone up to 18.8-fold (P<0.001). EMP1 silencing also abrogated migration and adhesion to mesenchymal stromal cells (MSCs) by 78.3±9.0 and 29.3±4.1% compared with shNSC (P<0.05). We discovered that EMP1 contributes to MSC-mediated prednisolone resistance. Pathway analysis indicated that EMP1 signals through the Src kinase family. EMP1-high BCP-ALL patients showed a poorer 5-year event-free survival compared with EMP1-low patients (77±2 vs 89±2%, P=0.003). Multivariate analysis taking along white blood cell count, age, prednisolone resistance and subtype identified EMP1 as an independent predictor for poor outcome in BCP-ALL (P=0.004, hazard ratio: 2.36 (1.31-4.25). This study provides preclinical evidence that EMP1 is an interesting candidate for drug development to optimize treatment of BCP-ALL.Leukemia advance online publication, 14 March 2014; doi:10.1038/leu.2014.80. | 24625531
 |
Inhibitory effect of natural anti-inflammatory compounds on cytokines released by chronic venous disease patient-derived endothelial cells.
Tisato, V; Zauli, G; Rimondi, E; Gianesini, S; Brunelli, L; Menegatti, E; Zamboni, P; Secchiero, P
Mediators of inflammation
2013
423407
2013
概要を表示する
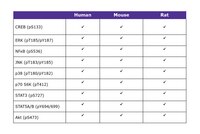
Large vein endothelium plays important roles in clinical diseases such as chronic venous disease (CVD) and thrombosis; thus to characterize CVD vein endothelial cells (VEC) has a strategic role in identifying specific therapeutic targets. On these bases we evaluated the effect of the natural anti-inflammatory compounds α-Lipoic acid and Ginkgoselect phytosome on cytokines/chemokines released by CVD patient-derived VEC. For this purpose, we characterized the levels of a panel of cytokines/chemokines (n = 31) in CVD patients' plasma compared to healthy controls and their release by VEC purified from the same patients, in unstimulated and TNF-α stimulated conditions. Among the cytokines/chemokines released by VEC, which recapitulated the systemic profile (IL-8, TNF-α, GM-CSF, INF- α2, G-CSF, MIP-1β, VEGF, EGF, Eotaxin, MCP-1, CXCL10, PDGF, and RANTES), we identified those targeted by ex vivo treatment with α-Lipoic acid and/or Ginkgoselect phytosome (GM-CSF, G-CSF, CXCL10, PDGF, and RANTES). Finally, by investigating the intracellular pathways involved in promoting the VEC release of cytokines/chemokines, which are targeted by natural anti-inflammatory compounds, we documented that αLipoic acid significantly counteracted TNF-α-induced NF-κB and p38/MAPK activation while the effects of Ginkgo biloba appeared to be predominantly mediated by Akt. Our data provide new insights into the molecular mechanisms of CVD pathogenesis, highlighting new potential therapeutic targets. | 24489443
 |
Lipopolysaccharide-binding protein inhibits toll-like receptor 2 activation by lipoteichoic acid in human odontoblast-like cells.
Carrouel, F; Staquet, MJ; Keller, JF; Baudouin, C; Msika, P; Bleicher, F; Alliot-Licht, B; Farges, JC
Journal of Endodontics
39
1008-14
2013
概要を表示する
Previous studies have suggested that odontoblasts sense gram-positive bacteria components through Toll-like receptor 2 (TLR2) and trigger dental pulp immunity by producing proinflammatory cytokines. Currently, the factors that modulate odontoblast TLR2 activation are unknown. Our aim was to investigate lipopolysaccharide-binding protein (LBP) effects on the TLR2-mediated odontoblast response.Human odontoblast-like cells were stimulated with lipoteichoic acid (LTA) (a TLR2 ligand), LBP, CD14 (a TLR2 cofactor), or various combinations of LTA/LBP, LTA/CD14, or LTA/CD14/LBP. CXCL8, IL6, and TLR2 gene expression was assessed by real-time polymerase chain reaction. CXCL8 and interleukin (IL)-6 production was determined by enzyme-linked immunosorbent assay in culture supernatants of cells stimulated with LTA, LTA/CD14, or LTA/CD14/LBP. LBP effects on nuclear factor kappa B (NF-κB), p38, JNK, ERK, STAT3, and p70S6 signaling pathways were determined in LTA-stimulated odontoblast-like cells with a multiplex biometric immunoassay. LBP effects were compared with specific inhibitors of these signaling pathways. LBP transcript and protein were investigated in vivo in healthy and inflamed dental pulps by real-time polymerase chain reaction and immunohistochemistry.Activation of CXCL8, IL6, and TLR2 gene expression and CXCL8 and IL-6 secretion in LTA- and LTA/CD14-stimulated odontoblast-like cells was significantly decreased by LBP. LBP inhibited NF-κB and p38 signaling pathways in LTA-stimulated cells in a similar way to NF-κB and p38 inhibitors. LBP transcript and protein were detected in vivo in inflamed dental pulps but not in healthy ones.These results demonstrate that LBP reduces TLR2-dependent production of inflammatory cytokines by odontoblast-like cells. We suggest that in this way it could modulate host defense in human dental pulp. | 23880268
 |