Maritoclax induces apoptosis in acute myeloid leukemia cells with elevated Mcl-1 expression.
Doi, K; Liu, Q; Gowda, K; Barth, BM; Claxton, D; Amin, S; Loughran, TP; Wang, HG
Cancer biology & therapy
15
1077-86
2014
概要を表示する
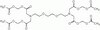
Acute myeloid leukemia (AML) is one of the deadliest leukemias for which there is an urgent and unmet need for the development of novel treatment strategies. Multiple drug resistance mechanisms mediate poor drug response and relapse in patients, and a selective Mcl-1 inhibitor has been speculated to be a promising agent in the treatment of AML. Here, we describe that maritoclax, a small molecule Mcl-1 inhibitor, induces Mcl-1 proteasomal degradation without transcriptional downregulation. Maritoclax killed AML cell lines and primary cells with elevated Mcl-1 levels through selective Mcl-1 downregulation, and synergized with ABT-737 to overcome Mcl-1-mediated ABT-737 resistance. Maritoclax was more effective than daunorubicin at inducing leukemic cell death when co-cultured with HS-5 bone marrow stroma cells, while being less toxic than daunorubicin against HS-5 stroma cells, primary mouse bone marrow cells, and hematopoietic progenitor cells. Moreover, maritoclax administration at 20 mg/kg/d intraperitoneally caused significant U937 tumor shrinkage, as well as 36% tumors remission rate in athymic nude mice, without apparent toxicity to healthy tissue or circulating blood cells. In summary, our studies suggest that maritoclax belongs to a novel class of Mcl-1 inhibitors that has the potential to be developed for the treatment of AML. | 24842334
 |
Integrative genomic and transcriptomic analysis identified candidate genes implicated in the pathogenesis of hepatosplenic T-cell lymphoma.
Finalet Ferreiro, J; Rouhigharabaei, L; Urbankova, H; van der Krogt, JA; Michaux, L; Shetty, S; Krenacs, L; Tousseyn, T; De Paepe, P; Uyttebroeck, A; Verhoef, G; Taghon, T; Vandenberghe, P; Cools, J; Wlodarska, I
PloS one
9
e102977
2014
概要を表示する
Hepatosplenic T-cell lymphoma (HSTL) is an aggressive lymphoma cytogenetically characterized by isochromosome 7q [i(7)(q10)], of which the molecular consequences remain unknown. We report here results of an integrative genomic and transcriptomic (expression microarray and RNA-sequencing) study of six i(7)(q10)-positive HSTL cases, including HSTL-derived cell line (DERL-2), and three cases with ring 7 [r(7)], the recently identified rare variant aberration. Using high resolution array CGH, we profiled all cases and mapped the common deleted region (CDR) at 7p22.1p14.1 (34.88 Mb; 3506316-38406226 bp) and the common gained region (CGR) at 7q22.11q31.1 (38.77 Mb; 86259620-124892276 bp). Interestingly, CDR spans a smaller region of 13 Mb (86259620-99271246 bp) constantly amplified in cases with r(7). In addition, we found that TCRG (7p14.1) and TCRB (7q32) are involved in formation of r(7), which seems to be a byproduct of illegitimate somatic rearrangement of both loci. Further transcriptomic analysis has not identified any CDR-related candidate tumor suppressor gene. Instead, loss of 7p22.1p14.1 correlated with an enhanced expression of CHN2 (7p14.1) and the encoded β2-chimerin. Gain and amplification of 7q22.11q31.1 are associated with an increased expression of several genes postulated to be implicated in cancer, including RUNDC3B, PPP1R9A and ABCB1, a known multidrug resistance gene. RNA-sequencing did not identify any disease-defining mutation or gene fusion. Thus, chromosome 7 imbalances remain the only driver events detected in this tumor. We hypothesize that the Δ7p22.1p14.1-associated enhanced expression of CHN2/β2-chimerin leads to downmodulation of the NFAT pathway and a proliferative response, while upregulation of the CGR-related genes provides growth advantage for neoplastic δγT-cells and underlies their intrinsic chemoresistance. Finally, our study confirms the previously described gene expression profile of HSTL and identifies a set of 24 genes, including three located on chromosome 7 (CHN2, ABCB1 and PPP1R9A), distinguishing HSTL from other malignancies. | 25057852
 |
In vitro drug response and efflux transporters associated with drug resistance in pediatric high grade glioma and diffuse intrinsic pontine glioma.
Veringa, SJ; Biesmans, D; van Vuurden, DG; Jansen, MH; Wedekind, LE; Horsman, I; Wesseling, P; Vandertop, WP; Noske, DP; Kaspers, GJ; Hulleman, E
PloS one
8
e61512
2013
概要を表示する
Pediatric high-grade gliomas (pHGG), including diffuse intrinsic pontine gliomas (DIPG), are the leading cause of cancer-related death in children. While it is clear that surgery (if possible), and radiotherapy are beneficial for treatment, the role of chemotherapy for these tumors is still unclear. Therefore, we performed an in vitro drug screen on primary glioma cells, including three DIPG cultures, to determine drug sensitivity of these tumours, without the possible confounding effect of insufficient drug delivery. This screen revealed a high in vitro cytotoxicity for melphalan, doxorubicine, mitoxantrone, and BCNU, and for the novel, targeted agents vandetanib and bortezomib in pHGG and DIPG cells. We subsequently determined the expression of the drug efflux transporters P-gp, BCRP1, and MRP1 in glioma cultures and their corresponding tumor tissues. Results indicate the presence of P-gp, MRP1 and BCRP1 in the tumor vasculature, and expression of MRP1 in the glioma cells themselves. Our results show that pediatric glioma and DIPG tumors per se are not resistant to chemotherapy. Treatment failure observed in clinical trials, may rather be contributed to the presence of drug efflux transporters that constitute a first line of drug resistance located at the blood-brain barrier or other resistance mechanism. As such, we suggest that alternative ways of drug delivery may offer new possibilities for the treatment of pediatric high-grade glioma patients, and DIPG in particular. | 23637844
 |
Multidrug Resistance Gene (MDR-1) and Risk of Brain Metastasis in Epithelial Ovarian, Fallopian Tube, and Peritoneal Cancer.
Matsuo K, Eno ML, Ahn EH, Shahzad MM, Im DD, Rosenshein NB, Sood AK
Am J Clin Oncol
2010
概要を表示する
BACKGROUND: To evaluate risk factors that predict brain metastasis in epithelial ovarian, fallopian tube, and peritoneal cancer. | 20921883
 |
Co-expression of MDR-associated markers, including P-170, MRP and LRP and cytoskeletal proteins, in three resistant variants of the human ovarian carcinoma cell line, OAW42
Moran, E. et al.
Eur. J. Cancer , 33:652-660 (1997)
1997
| 9274450
 |
Sequential assessment of multidrug resistance phenotype and measurement of S-phase fraction as predictive markers of breast cancer response to neoadjuvant chemotherapy
Chevillard, S. et al.
Cancer , 77:292-300 (1996)
1996
| 8625237
 |
Multidrug resistance P-glycoprotein monoclonal antibody JSB-1 crossreacts with pyruvate carboxylase
Rao, V V, et al
J Histochem Cytochem, 43:1187-1192 (1995)
1995
| 8537634
 |
Expression of P-glycoprotein in high-grade osteosarcomas in relation to clinical outcome
Baldini, N. et al.
New Engl. J. Med. , 333:1380-1385 (1995)
1995
| 7477118
 |
New immunohistochemical "sandwich" staining method for mdr1 P-glycoprotein detection with JSB-1 monoclonal antibody in formalin-fixed, paraffin-embedded human tissues
Toth, K. et al.
Am. J. Pathol, 144:227-236 (1994)
1994
| 7508682
 |
Immunohistochemical study of expression and cellular localization of the multidrug resistance gene product P-glycoprotein in primary liver carcinoma
Itsubo, M. et al.
Cancer , 73:298-303 (1994)
1994
| 7904895
 |