The endothelial microenvironment in the venous valvular sinus: thromboresistance trends and inter-individual variation.
Trotman, WE; Taatjes, DJ; Callas, PW; Bovill, EG
Histochem Cell Biol
135
141-52
2010
Afficher le résumé
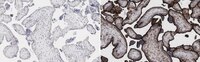
The valve sinuses of the deep venous system are frequent sites of venous thrombus initiation. We previously reported that, in comparison with the non-valvular lumenal endothelium, the valve sinus endothelium had decreased expression of von Willebrand factor (vWF) and increased expression of endothelial protein C receptor (EPCR) and thrombomodulin (TM), suggesting alteration in the procoagulant/anticoagulant balance. We hypothesized that increased stasis in the deeper recesses of the venous valves would be associated with a gradient of increased thromboresistance. Expression of EPCR, TM, and vWF was analyzed via quantitative confocal immunofluorescence in residual saphenous veins collected following coronary artery bypass procedures. In agreement with our hypothesis, endothelial expression of vWF in the valve sinus decreased from the uppermost to the deepest region of the valve sinus. In contrast to our hypothesis, EPCR expression decreased from the uppermost to the deepest region of the valve sinus (p < 0.001) and TM expression remained unchanged throughout the valve sinus. Comparison of the non-valvular lumenal endothelium with the valve sinus endothelium demonstrated significantly decreased vWF expression (p < 0.001) in the valvular sinus consistent with our previous report; however, we did not observe statistically significant differences in EPCR or TM expression in this comparison. In addition, remarkable inter-individual variation in expression of these three proteins was also observed. These findings suggest that the genesis of these observations is more complex than predicted by our initial hypothesis, likely due, at least in part, to the complex rheology of the valvular sinus microenvironment. | 21298440
 |
Cellular regulation of blood coagulation: a model for venous stasis.
Campbell, JE; Brummel-Ziedins, KE; Butenas, S; Mann, KG
Blood
116
6082-91
2009
Afficher le résumé
We have adapted the corn-trypsin inhibitor whole-blood model to include EA.hy926 as an endothelium surrogate to evaluate the vascular modulation of blood coagulation initiated by relipidated recombinant tissue factor (rTf) and a cellular Tf surrogate, lipopolysaccharide (LPS)-stimulated THP1 cells (LPS-THP-1). Compared with bare tubes, EA.hy926 with rTf decreased the rate of thrombin formation, ITS accumulation, and the production of fibrinopeptide A. These phenomena occurred with increased rates of factor Va (fVa) inactivation by cleavages at R(506) and R(306). Thus, EA.hy926 provides thrombin-dependent protein C activation and APC fVa inactivation. Comparisons of rTf with LPS-THP-1 showed that the latter gave reduced rates for TAT formation but equivalent fibrinopeptide A, and fV activation/inactivation. In the presence of EA.hy926, the reverse was obtained; with the surrogate endothelium and LPS-THP-1 the rates of TAT generation, fibrinopeptide release, and fV activation were almost doubled, whereas cleavage at R(306) was equivalent. These observations suggest cooperativity between the 2 cell surrogates. These data suggest that the use of these 2 cell lines provides a reproducible quasi-endothelial quasi-inflammatory cytokine-stimulated monocyte system that provides a method to evaluate the variations in blood phenotype against the background of stable inflammatory cell activator and a stable vascular endothelial surrogate. | 20864579
 |
Effects of the chemotherapeutic agent doxorubicin on the protein C anticoagulant pathway.
Woodley-Cook, J; Shin, LY; Swystun, L; Caruso, S; Beaudin, S; Liaw, PC
Mol Cancer Ther
5
3303-11
2005
Afficher le résumé
Although chemotherapy treatment is associated with an increased risk of thrombosis, the pathogenic mechanisms for the thrombogenic effect of chemotherapeutic drugs are poorly understood. We hypothesize that exposure of vascular endothelial cells to chemotherapeutic agents results in the loss of a thromboresistant phenotype. In this study, we examined the effects of the chemotherapeutic agent doxorubicin on the endothelium-based protein C anticoagulant pathway. The endothelial cell protein C receptor (EPCR) and thrombomodulin are two endothelial cell surface receptors required for the conversion of zymogen protein C to the anticoagulant enzyme activated protein C. Exposure of human umbilical vein endothelial cells (HUVEC) to doxorubicin resulted in a dose- and time-dependent decrease in cell surface EPCR levels. This decrease occurred as a result of receptor shedding as well as from a down-regulation in EPCR mRNA levels. In contrast, doxorubicin treatment of HUVECs resulted in a dose- and time-dependent increase in cell surface thrombomodulin attributed to an up-regulation of thrombomodulin mRNA levels. The net effect of the doxorubicin-induced changes in EPCR and thrombomodulin levels was a decrease in the capacity of HUVECs to convert protein C to activated protein C. Preliminary studies suggest that doxorubicin free radical metabolites mediate the doxorubicin-induced changes in EPCR expression but not those of thrombomodulin expression. In summary, these results suggest that doxorubicin alters the hemostatic balance of endothelial cells by down-regulating the endothelium-based protein C anticoagulant pathway. | 17172434
 |
Reconstitution of the human endothelial cell protein C receptor with thrombomodulin in phosphatidylcholine vesicles enhances protein C activation.
Xu, J; Esmon, NL; Esmon, CT
J Biol Chem
274
6704-10
1998
Afficher le résumé
Blocking protein C binding to the endothelial cell protein C receptor (EPCR) on the endothelium is known to reduce protein C activation rates. Now we isolate human EPCR and thrombomodulin (TM) and reconstitute them into phosphatidylcholine vesicles. The EPCR increases protein C activation rates in a concentration-dependent fashion that does not saturate at 14 EPCR molecules/TM. Without EPCR, the protein C concentration dependence fits a single class of sites (Km = 2.17 +/- 0.13 microM). With EPCR, two classes of sites are apparent (Km = 20 +/- 15 nM and Km = 3.2 +/- 1.7 microM). Increasing the EPCR concentration at a constant TM concentration increases the percentage of high affinity sites. Holding the TM:EPCR ratio constant while decreasing the density of these proteins results in a decrease in the EPCR enhancement of protein C activation, suggesting that there is little affinity of the EPCR for TM. Negatively charged phospholipids also enhance protein C activation. EPCR acceleration of protein C activation is blocked by anti-EPCR antibodies, but not by annexin V, whereas the reverse is true with negatively charged phospholipids. Human umbilical cord endothelium expresses approximately 7 times more EPCR than TM. Anti-EPCR antibody reduces protein C activation rates 7-fold over these cells, whereas annexin V is ineffective, indicating that EPCR rather than negatively charged phospholipid provide the surface for protein C activation. EPCR expression varies dramatically among vascular beds. The present results indicate that the EPCR concentration will determine the effectiveness of the protein C activation complex. | 10037768
 |
The endothelial cell protein C receptor augments protein C activation by the thrombin-thrombomodulin complex.
Stearns-Kurosawa, DJ; Kurosawa, S; Mollica, JS; Ferrell, GL; Esmon, CT
Proc Natl Acad Sci U S A
93
10212-6
1996
Afficher le résumé
Protein C activation on the surface of the endothelium is critical to the negative regulation of blood coagulation. We now demonstrate that monoclonal antibodies that block protein C binding to the endothelial cell protein C receptor (EPCR) reduce protein C activation rates by the thrombin-thrombomodulin complex on endothelium, but that antibodies that bind to EPCR without blocking protein C binding have no effect. The kinetic result of blocking the EPCR-protein C interaction is an increased apparent Km for the activation without altering the affinity of thrombin for thrombomodulin. Activation rates of the protein C derivative lacking the gamma-carboxyglutamic acid domain, which is required for binding to EPCR, are not altered by the anti-EPCR antibodies. These data indicate that the protein C activation complex involves protein C, thrombin, thrombomodulin, and EPCR. These observations open new questions about the control of coagulation reactions on vascular endothelium. | 8816778
 |