Hypoxic preconditioning of human mesenchymal stem cells overcomes hypoxia-induced inhibition of osteogenic differentiation.
Elias Volkmer,Bobby Cherian Kallukalam,Josef Maertz,Sven Otto,Inga Drosse,Hans Polzer,Wolfgang Bocker,Michael Stengele,Denitsa Docheva,Wolf Mutschler,Matthias Schieker
Tissue engineering. Part A
16
2009
Mostrar resumen
Osteogenic differentiation of human mesenchymal stem cells (hMSCs) into osteoblasts is a prerequisite for subsequent bone formation. Numerous studies have explored osteogenic differentiation under standard tissue culture conditions, which usually employ 21% of oxygen. However, bone precursor cells such as hMSCs reside in stem cell niches of low-oxygen atmospheres. Furthermore, they are subjected to low oxygen concentrations when cultured on three-dimensional scaffolds in vitro, and even more so after transplantation when vascularization has yet to be established. Similarly, hMSCs are exposed to low oxygen in the fracture microenvironment following bony injury. Recent studies revealed that hypoxic preconditioning improves cellular engraftment and survival in low-oxygen atmospheres. In our study we investigated the osteogenic differentiation potential of hMSCs under 2% O(2) (hypoxia) in comparison to a standard tissue culture oxygen atmosphere of 21% (normoxia). We assessed the osteogenic differentiation of hMSCs following hypoxic preconditioning to address whether this pretreatment is beneficial for subsequent differentiation processes as well. To validate our findings we carefully characterized the extent of hypoxia exerted and its effect on cell survival and proliferation. We found that hMSCs proliferate better if cultured under 2% of oxygen. We confirmed that osteogenic differentiation of hMSCs is indeed inhibited if osteogenic induction is carried out under constant hypoxia. Finally, we showed for the first time that hypoxic preconditioning of hMSCs prior to osteogenic induction restores osteogenic differentiation of hMSCs under hypoxic conditions. Collectively, our results indicate that maintaining constant levels of oxygen improves the osteogenic potential of hMSCs and suggest that low oxygen concentrations may preserve the stemness of hMSCs. In addition, our data support the hypothesis that if low-oxygen atmospheres are expected at the site of implantation, hypoxic pretreatment may be beneficial for the cells' subsequent in vivo performance. | 19642854
 |
Involvement of Hif-1 in desferrioxamine-induced invasion of glioblastoma cells.
Anja Elstner,Nikola Holtkamp,Andreas von Deimling
Clinical & experimental metastasis
24
2007
Mostrar resumen
Glioblastoma multiforme are highly invasive brain tumors. Experimental approaches focus on unravelling the mechanisms of invasion, this being a major reason for the poor prognosis of these tumors. Our previous results hinted towards involvement of the iron metabolism in invasion. In this study, we examined the effect of iron depletion on the invasive phenotype of glioblastoma cells. Transwell Matrigel invasion assays were used to monitor iron-dependent invasion of human glioblastoma cell lines U373MG and DBTRG05MG. Intracellular iron concentrations were modulated by applying desferrioxamine (DFO) and ferric ammonium citrate (FAC). We detected enhanced invasion of glioblastoma cells upon DFO-induced iron depletion. Treatment of cells with FAC strongly inhibited invasion. DFO treatment resulted in hypoxia-inducible factor 1 (Hif-1)-mediated induction of urokinase plasminogen activator receptor and matrix metalloproteinase 2. Further, RNA interference-mediated repression of urokinase plasminogen activator receptor inhibited DFO-induced invasion. Our data demonstrate a direct effect of DFO on Hif-1 expression resulting in activation of factors associated with ECM degradation and invasion of glioma cells. These findings caution on utilization of DFO and other iron chelators in the treatment of tumors with invasive potential. | 17357815
 |
Differentiation of human embryonic stem cells to dopaminergic neurons in serum-free suspension culture.
Thomas C Schulz, Scott A Noggle, Gail M Palmarini, Deb A Weiler, Ian G Lyons, Kate A Pensa, Adrian C B Meedeniya, Bruce P Davidson, Nevin A Lambert, Brian G Condie
Stem cells (Dayton, Ohio)
22
1218-38
2004
Mostrar resumen
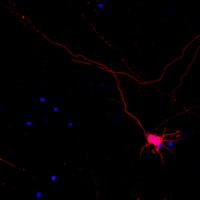
The use of human embryonic stem cells (hESCs) as a source of dopaminergic neurons for Parkinson's disease cell therapy will require the development of simple and reliable cell differentiation protocols. The use of cell cocultures, added extracellular signaling factors, or transgenic approaches to drive hESC differentiation could lead to additional regulatory as well as cell production delays for these therapies. Because the neuronal cell lineage seems to require limited or no signaling for its formation, we tested the ability of hESCs to differentiate to form dopamine-producing neurons in a simple serum-free suspension culture system. BG01 and BG03 hESCs were differentiated as suspension aggregates, and neural progenitors and neurons were detectable after 2-4 weeks. Plated neurons responded appropriately to electrophysiological cues. This differentiation was inhibited by early exposure to bone morphogenic protein (BMP)-4, but a pulse of BMP-4 from days 5 to 9 caused induction of peripheral neuronal differentiation. Real-time polymerase chain reaction and whole-mount immunocytochemistry demonstrated the expression of multiple markers of the midbrain dopaminergic phenotype in serum-free differentiations. Neurons expressing tyrosine hydroxylase (TH) were killed by 6-hydroxydopamine (6-OHDA), a neurotoxic catecholamine. Upon plating, these cells released dopamine and other catecholamines in response to K+ depolarization. Surviving TH+ neurons, derived from the cells differentiated in serum-free suspension cultures, were detected 8 weeks after transplantation into 6-OHDA-lesioned rat brains. This work suggests that hESCs can differentiate in simple serum-free suspension cultures to produce the large number of cells required for transplantation studies. | 15579641
 |