Expression of leukocyte adhesion molecules in human subfoveal choroidal neovascular membranes treated with and without photodynamic therapy.
Deborah C Yeh, Deisy V Bula, Joan W Miller, Evangelos S Gragoudas, Jorge G Arroyo
Investigative ophthalmology visual science
45
2368-73
2004
Kivonat megmutatása
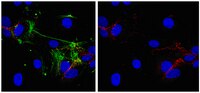
PURPOSE: The purposes of this study were to investigate the immunostaining of the leukocyte adhesion molecules intercellular adhesion molecule (ICAM)-1 and E-selectin in subfoveal choroidal neovascular membranes (CNVMs) surgically excised from patients with age-related macular degeneration (AMD) and to determine whether prior photodynamic therapy (PDT) alters their immunostaining. METHODS: The localization of ICAM-1 and E-selectin in 10 subfoveal CNVMs was determined by immunohistochemistry. Membranes were also immunostained for CD31 to assess vascularity. RESULTS: Significantly higher numbers of CD31-staining vessels per unit membrane area were found in the peripheral regions of the membranes compared with the central regions (P = 0.05). ICAM-1 immunoreactivity in the CNVMs was found predominantly on RPE cells, but also on small vessels in the periphery. ICAM-1 staining was significantly more intense in the peripheral, more cellular areas of the membranes than in the central, more fibrotic regions (P = 0.04). ICAM-1 staining in the periphery of the CNVMs was greater than that in choroidal vessels and the RPE of the normal control eye. ICAM-1 immunostaining grade in peripheral regions of the CNVMs decreased with the increasing number of PDT treatments (P = 0.05). Some of the CNVMs also stained for E-selectin in RPE cells and small vessels in the periphery. CONCLUSIONS: In subfoveal CNVMs from patients with AMD, there is increased immunostaining for leukocyte adhesion molecules, particularly in the peripheral, more cellular regions where angiogenesis may be ongoing. Increasing numbers of PDT treatments may be associated with decreased ICAM-1 immunostaining in the proliferating edges of the CNVMs. | 15223819
 |
Neutrality of the canonical NF-kappaB-dependent pathway for human and murine cytomegalovirus transcription and replication in vitro.
Chris A Benedict, Ana Angulo, Ginelle Patterson, Sukwon Ha, Huang Huang, Martin Messerle, Carl F Ware, Peter Ghazal
Journal of virology
78
741-50
2004
Kivonat megmutatása
Cytomegalovirus (CMV) is known to rapidly induce activation of nuclear factor kappaB (NF-kappaB) after infection of fibroblast and macrophage cells. NF-kappaB response elements are present in the enhancer region of the CMV major immediate-early promoter (MIEP), and activity of the MIEP is strongly upregulated by NF-kappaB in transient-transfection assays. Here we investigate whether the NF-kappaB-dependent pathway is required for initiating or potentiating human and murine CMV replication in vitro. We show that expression of a dominant negative mutant of the inhibitor of NF-kappaB-alpha (IkappaBalphaM) does not alter the replication kinetics of human or mouse CMV in cultured cells. In addition, mouse embryo fibroblasts genetically deficient for p65/RelA actually showed elevated levels of MCMV replication. Mutation of all NF-kappaB response elements within the enhancer of the MIEP in a recombinant mouse CMV containing the human MIEP (hMCMV-ES), which we have previously shown to replicate in murine fibroblasts with kinetics equivalent to that of wild-type mouse CMV, did not negatively affect replication in fibroblasts. Taken together, these data show that, for CMV replication in cultured fibroblasts activation of the canonical NF-kappaB pathway and binding of NF-kappaB to the MIEP are dispensable, and in the case of p65 may even interfere, thus uncovering a previously unrecognized level of complexity in the host regulatory network governing MIE gene expression in the context of a viral infection. Teljes cikk | 14694106
 |