Impact of cigarette smoke extract and hyperglycemic conditions on blood-brain barrier endothelial cells.
Prasad, S; Sajja, RK; Park, JH; Naik, P; Kaisar, MA; Cucullo, L
Fluids and barriers of the CNS
12
18
2015
显示摘要
Diabetes and tobacco smoking are significant public health concerns which have been shown to independently impact the blood-brain barrier (BBB). Since smoking is a risk factor for diabetes and shares some of the common pathological pathways leading to metabolic abnormalities, it is hypothesized that their combination would produce additive or synergistic BBB dysfunction. Therefore, the objective of this study was to assess this hypothesis and evaluate the magnitude of these effects in vitro using hCMEC/D3 cells; a well-established human BBB endothelial cell line.Monolayers of hCMEC/D3 cells were exposed to hyperglycemic conditions (HG; 35 mM) or 5% soluble cigarette smoke extracts (CSE, model of mainstream smoke exposure) for 12-24 h. Cells were then harvested for subsequent biochemical analyses. Transendothelial electrical resistance (TEER) and paracellular permeability to florescent dextrans were used to assess monolayer integrity. Analysis of released factors and cytokines was carried out by ELISA. Western blot (WB) analysis/immunofluorescence of relevant molecular targets was carried out. P-gp efflux activity was measured using rhodamine 123.Immunofluorescence and WB data showed a significant ZO-1 down-regulation by HG and/or CSE over 24 h exposure. CSE in presence of HG produced a synergistic increase in release of vascular endothelial growth factor that was accompanied by decreased TEER and augmented permeability to labeled dextrans in a size-dependent manner. Moreover, CSE increased the expression of GLUT-1 and SGLT-1 in isolated membrane fractions of hCMEC/D3 cells. The effect was amplified by HG. Both, HG and CSE elicited the membrane upregulation of P-glycoprotein (P-gp) expression which however, was not paralleled by a comparable efflux activity. Interestingly, concomitant exposure to HG and CSE evoked a marked upregulation of PECAM-1 and other pro-inflammatory markers including IL-6 and -8, when compared to each condition alone. Moreover, exposure to all tested conditions amplified (to a different degree) cellular oxidative stress response denoted by increased Nrf2 nuclear translocation.Overall, our results have clearly shown an additive pattern in the release of angiogenic and inflammatory factors following concomitant exposure to HG and CSE. This suggests the involvement of common key modulators in BBB impairment by both CS and HG possibly through the activation of oxidative stress responses. | 26206552
 |
Endotoxin-induced inflammation down-regulates L-type amino acid transporter 1 (LAT1) expression at the blood-brain barrier of male rats and mice.
Wittmann, G; Mohácsik, P; Balkhi, MY; Gereben, B; Lechan, RM
Fluids and barriers of the CNS
12
21
2015
显示摘要
We recently reported that bacterial lipopolysaccharide (LPS)-induced inflammation decreases the expression of the primary thyroid hormone transporters at the blood-brain barrier, organic anion-transporting polypeptide 1c1 (OATP1c1) and monocarboxylate transporter 8 (MCT8). L-type amino acid transporters 1 and 2 (LAT1 & LAT2) are regarded as secondary thyroid hormone transporters, and are expressed in cells of the blood-brain or blood-cerebrospinal fluid barrier and by neurons. The purpose of this study was to examine the effect of LPS-induced inflammation on the expression of LAT1 and LAT2, as these may compensate for the downregulation of OATP1c1 and MCT8.LPS (2.5 mg/kg body weight) was injected intraperitoneally to adult, male, Sprague-Dawley rats and C57Bl/6 mice, which were euthanized 2, 4, 9, 24 or 48 h later. LAT1 and LAT2 mRNA expression were studied on forebrain sections using semiquantitative radioactive in situ hybridization. LAT1 protein levels in brain vessels were studied using LAT1 immunofluorescence. Statistical comparisons were made by the non-parametric Kruskal-Wallis and Dunn's tests.In both species, LAT1 mRNA decreased in brain blood vessels as soon as 2 h after LPS injection and was virtually undetectable at 4 h and 9 h. During recovery from endotoxemia, 48 h after LPS injection, LAT1 mRNA in brain vessels increased above control levels. A modest but significant decrease in LAT1 protein levels was detected in the brain vessels of mice at 24 h following LPS injection. LPS did not affect LAT1 and LAT2 mRNA expression in neurons and choroid plexus epithelial cells.The results demonstrate that LPS-induced inflammation rapidly decreases LAT1 mRNA expression at the blood-brain barrier in a very similar manner to primary thyroid hormone transporters, while changes in LAT1 protein level follow a slower kinetics. The data raise the possibility that inflammation may similarly down-regulate other blood-brain barrier transport systems at the transcriptional level. Future studies are required to examine this possibility and the potential pathophysiological consequences of inflammation-induced changes in blood-brain barrier transport functions. | 26337286
 |
PET Demonstrates Functional Recovery after Treatment by Danhong Injection in a Rat Model of Cerebral Ischemic-Reperfusion Injury.
Wang, Z; Song, F; Li, J; Zhang, Y; He, Y; Yang, J; Zhou, H; Zhao, T; Fu, W; Xing, P; Wan, H; Tian, M; Zhang, H
Evidence-based complementary and alternative medicine : eCAM
2014
430757
2014
显示摘要
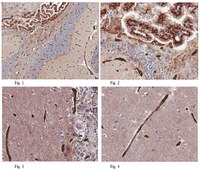
This study aimed to investigate neuroprotection of Danhong injection (DHI) in a rat model of cerebral ischemia using (18)F-fluorodeoxyglucose positron emission tomography ((18)F-FDG-PET). Method. Rats were divided into 5 groups: sham group, ischemia-reperfusion untreated (IRU) group, DHI-1 group (DHI 1 mL/kg/d), DHI-2 group (DHI 2 mL/kg/d), and DHI-4 group (DHI 4 mL/kg/d). AII the treated groups were intraperitoneally injected with DHI daily for 14 days. The therapeutic effects in terms of cerebral infarct volume, neurological function, and cerebral glucose metabolism were evaluated. Expression of TNF-α and IL-1β was detected with enzyme-linked immunosorbent assay (ELISA). Levels of mature neuronal marker (NeuN), glial marker (GFAP), vascular density factor (vWF), and glucose transporter 1 (GLUT1) were assessed by immunohistochemistry. Results. Compared with the IRU group, rats treated with DHI showed dose dependent reductions in cerebral infarct volume and levels of proinflammatory cytokines, improvement of neurological function, and recovery of cerebral glucose metabolism. Meanwhile, the significantly increased numbers of neurons, gliocytes, and vessels and the recovery of glucose utilization were found in the peri-infarct region after DHI treatment using immunohistochemical analysis. Conclusion. This study demonstrated the metabolic recovery after DHI treatment by micro-PET imaging with (18)F-FDG and the neuroprotective effects of DHI in a rat model of cerebral ischemic-reperfusion injury. | 24707308
 |













 Antibody[191012-ALL].jpg)



