Maternal anti-platelet β3 integrins impair angiogenesis and cause intracranial hemorrhage.
Yougbaré, I; Lang, S; Yang, H; Chen, P; Zhao, X; Tai, WS; Zdravic, D; Vadasz, B; Li, C; Piran, S; Marshall, A; Zhu, G; Tiller, H; Killie, MK; Boyd, S; Leong-Poi, H; Wen, XY; Skogen, B; Adamson, SL; Freedman, J; Ni, H
The Journal of clinical investigation
125
1545-56
2015
Afficher le résumé
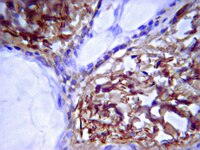
Fetal and neonatal alloimmune thrombocytopenia (FNAIT) is a life-threatening disease in which intracranial hemorrhage (ICH) is the major risk. Although thrombocytopenia, which is caused by maternal antibodies against β3 integrin and occasionally by maternal antibodies against other platelet antigens, such as glycoprotein GPIbα, has long been assumed to be the cause of bleeding, the mechanism of ICH has not been adequately explored. Utilizing murine models of FNAIT and a high-frequency ultrasound imaging system, we found that ICH only occurred in fetuses and neonates with anti-β3 integrin-mediated, but not anti-GPIbα-mediated, FNAIT, despite similar thrombocytopenia in both groups. Only anti-β3 integrin-mediated FNAIT reduced brain and retina vessel density, impaired angiogenic signaling, and increased endothelial cell apoptosis, all of which were abrogated by maternal administration of intravenous immunoglobulin (IVIG). ICH and impairment of retinal angiogenesis were further reproduced in neonates by injection of anti-β3 integrin, but not anti-GPIbα antisera. Utilizing cultured human endothelial cells, we found that cell proliferation, network formation, and AKT phosphorylation were inhibited only by murine anti-β3 integrin antisera and human anti-HPA-1a IgG purified from mothers with FNAIT children. Our data suggest that fetal hemostasis is distinct and that impairment of angiogenesis rather than thrombocytopenia likely causes FNAIT-associated ICH. Additionally, our results indicate that maternal IVIG therapy can effectively prevent this devastating disorder. | 25774504
 |
Six-transmembrane epithelial antigen of the prostate (STEAP1 and STEAP2)-differentially expressed by murine and human mesenchymal stem cells.
Rasilaben J Vaghjiani,Sonia Talma,Christopher L Murphy
Tissue engineering. Part A
15
2009
Afficher le résumé
Mesenchymal stem cells (MSCs) have great potential for cell-based therapies. However, lack of cell-specific markers thwarts full realization of this as it prevents their identification in vivo, and subsequent purification. In the present study, to ensure cell purity multiple individual clones were derived from the bone marrow of BALB/b and BALB/c mice, and subsequently defined as MSCs by demonstrating their multipotentiality and self-renewal ability. In an effort to define the molecular signature of such MSCs and identify potentially cell-specific markers, an extensive genome-wide microarray analysis was performed comparing eight individual undifferentiated MSC clones to four different controls-corresponding differentiated MSC clones, bone marrow adherent cells, freshly isolated bone marrow cells, and embryonic fibroblasts. Strikingly, all MSC clones expressed differentially high levels of six-transmembrane epithelial antigen of the prostate (STEAP1 and STEAP2). Further, both STEAP members showed an extremely similar expression profile to stem cell antigen-1 (Sca-1) as demonstrated by two-dimensional hierarchical cluster analysis. Most importantly, differentially high levels of STEAP1 and STEAP2 proteins were also detected in human multipotent bone marrow adherent cultures. Thus, STEAPs may represent novel markers of MSCs in man as well as mice. Depletion of STEAP1 in human MSCs using RNAi resulted in decreased cell adhesion to tissue culture plastic. Further work is now needed to fully uncover its function in these cells, and to explore its potential as a marker of MSCs. | 19196137
 |
Six (or more) drugs in search of a mechanism: DNA methyltransferase and histone deacetylase inhibitors in the treatment of myelodysplastic syndromes.
Steven D Gore
Journal of the National Comprehensive Cancer Network : JNCCN
4
83-90
2005
Afficher le résumé
The clinical activity of the DNA methyltransferase inhibitors 5-azacitidine and 2'-deoxy-5-azacytidine in myelodysplastic syndromes (MDS) suggests that epigenetic modulation of gene transcription may play an important pathogenetic role in the development and expression of these diseases. Approximately 50% of patients treated with these compounds experience hematologic improvement, making these the most active single agents for unselected patients with MDS. Responses include complete and partial hematologic responses. Two randomized trials have shown that the use of these drugs significantly alters the natural history of MDS compared with supportive care. Histone deacetylase inhibitors, which may also impact the expression of genes through epigenetic mechanisms, seem to have measurable activity in MDS in preliminary studies. Histone deacetylase inhibitors are most likely used in combination with other agents, including DNA methyltransferase inhibitors. Despite the clinical activity of these classes of drugs, there is no conclusive evidence that their clinical activity is attributable to their impact on the epigenome. Such information will be critical in the development of more effective congeners and drug combinations in ongoing attempts to improve the outcome of patients with MDS. | 16403407
 |