Synergism of Human Amnion-derived Multipotent Progenitor (AMP) Cells and a Collagen Scaffold in Promoting Brain Wound Recovery: Pre-clinical Studies in an Experimental Model of Penetrating Ballistic-like Brain Injury.
Chen Z, Lu XC, Shear DA, Dave JR, Davis AR, Evangelista CA, Duffy D, Tortella FC
Brain Res
2009
Mostrar resumen
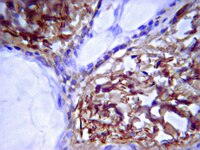
One of the histopathological consequences of a penetrating ballistic brain injury is the formation of a permanent cavity. In a previous study using the penetrating ballistic-like brain injury (PBBI) model, engrafted Human Amnion-derived Multipotent Progenitor (AMP) cells failed to survive when injected directly in the injury tract, suggesting that the cell survival requires a supportive matrix. In this study, we seated AMP cells in a collagen-based scaffold, injected into the injury core, and investigated cell survival and neuroprotection following PBBI. AMP cells suspended in AMP Cell Conditioned Medium (ACCS) or in a liquefied collagen matrix were injected immediately after a PBBI along the penetrating injury tract. Injured control rats received only liquefied collagen matrix. All animals were allowed to survive two weeks. Consistent with our previous results AMP cells suspended in ACCS failed to survive; likewise, no collagen was identified at the injury site when injected alone. In contrast, both AMP cells and the collagen were preserved in the injury cavity when injected together. In addition, AMP cells/collagen treatment preserved some apparent brain tissue in the injury cavity, and there was measurable infiltration of endogenous neural progenitor cells and astrocytes into the preserved brain tissue. AMP cells were also found to have migrated into the subventricular zone and the corpus callosum. Moreover, the AMP cell/collagen treatment significantly attenuated the PBBI-induced axonal degeneration in the corpus callosum and ipsilateral thalamus and improved motor impairment on rotarod performance. Overall, collagen-based scaffold provided a supportive matrix for AMP cell survival, migration, and neuroprotection. | 20951684
 |
Inhibition of neurotrophin receptor p75 intramembran proteolysis by gamma-secretase inhibitor reduces medulloblastoma spinal metastasis.
Xiaoji Wang,Min Cui,Lei Wang,XueHong Chen,Pan Xin
Biochemical and biophysical research communications
403
2009
Mostrar resumen
Medulloblastoma (MB) is the most devastating and common pediatric brain tumor. Tumor cells invading into surrounding tissue and disseminating through cerebrospinal fluid make treatment extremely difficult. Identifying the mechanisms of MB cells is therefore imperative for the development of novel treatments. A research group demonstrated recently that the multifunctional signaling protein neurotrophin receptor p75(NTR) is a central regulator for glioma invasion. ?-secretase mediated processing of the p75(NTR) is a major contributor to the highly invasive nature of malignant gliomas. In this study we examine the p75(NTR) expression and processing in medulloblastoma cells. Results show that p75(NTR) is a critical regulator of medulloblastoma spinal metastasis. ?-secretase inhibitor, which blocks p75(NTR) proteolytic processing, significantly abrogates p75(NTR) induced medulloblastoma migration and invasion in vitro and in vivo. This data suggests that p75(NTR) is also an important therapeutic target for MB. ?-secretase inhibitor may be a potentially effective clinical application for the treatment of medulloblastoma spinal metastasis. | 21073863
 |
Gamma-secretase represents a therapeutic target for the treatment of invasive glioma mediated by the p75 neurotrophin receptor.
LiMei Wang, Jennifer J Rahn, XueQing Lun, Beichen Sun, John J P Kelly, Samuel Weiss, Stephen M Robbins, Peter A Forsyth, Donna L Senger
PLoS biology
6
e289
2008
Mostrar resumen
The multifunctional signaling protein p75 neurotrophin receptor (p75(NTR)) is a central regulator and major contributor to the highly invasive nature of malignant gliomas. Here, we show that neurotrophin-dependent regulated intramembrane proteolysis (RIP) of p75(NTR) is required for p75(NTR)-mediated glioma invasion, and identify a previously unnamed process for targeted glioma therapy. Expression of cleavage-resistant chimeras of p75(NTR) or treatment of animals bearing p75(NTR)-positive intracranial tumors with clinically applicable gamma-secretase inhibitors resulted in dramatically decreased glioma invasion and prolonged survival. Importantly, proteolytic processing of p75(NTR) was observed in p75(NTR)-positive patient tumor specimens and brain tumor initiating cells. This work highlights the importance of p75(NTR) as a therapeutic target, suggesting that gamma-secretase inhibitors may have direct clinical application for the treatment of malignant glioma. Artículo Texto completo | 19067488
 |