Sources of cells that contribute to atherosclerotic intimal calcification: an in vivo genetic fate mapping study.
Naik, V; Leaf, EM; Hu, JH; Yang, HY; Nguyen, NB; Giachelli, CM; Speer, MY
Cardiovascular research
94
545-54
2012
Show Abstract
Vascular cartilaginous metaplasia and calcification are common in patients with atherosclerosis. However, sources of cells contributing to the development of this complication are currently unknown. In this study, we ascertained the origin of cells that give rise to cartilaginous and bony elements in atherosclerotic vessels.We utilized genetic fate mapping strategies to trace cells of smooth muscle (SM) origin via SM22α-Cre recombinase and Rosa26-LacZ Cre reporter alleles. In animals expressing both transgenes, co-existence within a single cell of β-galactosidase [marking cells originally derived from SM cells (SMCs)] with osteochondrogenic (Runx2/Cbfa1) or chondrocytic (Sox9, type II collagen) markers, along with simultaneous loss of SM lineage proteins, provides a strong evidence supporting reprogramming of SMCs towards osteochondrogenic or chondrocytic differentiation. Using this technique, we found that vascular SMCs accounted for ~80% of Runx2/Cbfa1-positive cells and almost all of type II collagen-positive cells (~98%) in atherosclerotic vessels of LDLr-/- and ApoE-/- mice. We also assessed contribution from bone marrow (BM)-derived cells via analysing vessels dissected from chimerical ApoE-/- mice transplanted with green fluorescence protein-expressing BM. Marrow-derived cells were found to account for ~20% of Runx2/Cbfa1-positive cells in calcified atherosclerotic vessels of ApoE-/- mice.Our results are the first to definitively identify cell sources attributable to atherosclerotic intimal calcification. SMCs were found to be a major contributor that reprogrammed its lineage towards osteochondrogenesis. Marrow-derived cells from the circulation also contributed significantly to the early osteochondrogenic differentiation in atherosclerotic vessels. | 22436847
 |
Vitalization of porous polyethylene (medpor(®)) with chondrocytes promotes early implant vascularization and incorporation into the host tissue.
Susanne Ehrmantraut,Andreas Naumann,Vivienne Willnecker,Stephanie Akinyemi,Christina Körbel,Claudia Scheuer,Andrea Meyer-Lindenberg,Michael D Menger,Matthias W Laschke
Tissue engineering. Part A
18
2012
Show Abstract
Porous polyethylene (Medpor(®)) is frequently used in craniofacial reconstructive surgery. The successful incorporation of this alloplastic biomaterial depends on adequate vascularization. Here, we analyzed whether the early vascularization of porous polyethylene can be accelerated by vitalization with human chondrocytes. For this purpose, small polyethylene samples were coated with platelet-rich plasma (PRP) or a suspension of PRP and human chondrocytes. Uncoated polyethylene samples served as controls. Subsequently, the samples were implanted into the dorsal skinfold chamber of CD-1 nude mice to repetitively analyze their vascularization and biocompatibility by means of intravital fluorescence microscopy. PRP-chondrocyte-coated polyethylene exhibited an accelerated and improved vascularization when compared with the other two groups. This was indicated by a significantly higher functional capillary density of the microvascular network developing around the implants. Moreover, a leukocyte-endothelial cell interaction was found in a physiological range at the implantation site of all three groups, demonstrating that the vitalization with PRP and chondrocytes did not affect the good biocompatibility of the alloplastic material. Additional histological, immunohistochemical, and in situ hybridization analyses revealed that the chondrocytes formed a bioprotective tissue layer, which prevented the accumulation of macrophages and foreign body giant cells on the polyethylene surface. These findings clearly indicate that vitalization of polyethylene with chondrocytes promotes early implant vascularization and incorporation into the host tissue and, thus, may be a promising approach that prevents postoperative complications such as implant extrusion, migration, and infection. | 22452340
 |
Genipin cross-linked fibrin hydrogels for in vitro human articular cartilage tissue-engineered regeneration.
Emma V Dare, May Griffith, Philippe Poitras, James A Kaupp, Stephen D Waldman, David J Carlsson, Geoffrey Dervin, Christine Mayoux, Maxwell T Hincke
Cells, tissues, organs
190
313-25
2009
Show Abstract
Our objective was to examine the potential of a genipin cross-linked human fibrin hydrogel system as a scaffold for articular cartilage tissue engineering. Human articular chondrocytes were incorporated into modified human fibrin gels and evaluated for mechanical properties, cell viability, gene expression, extracellular matrix production and subcutaneous biodegradation. Genipin, a naturally occurring compound used in the treatment of inflammation, was used as a cross-linker. Genipin cross-linking did not significantly affect cell viability, but significantly increased the dynamic compression and shear moduli of the hydrogel. The ratio of the change in collagen II versus collagen I expression increased more than 8-fold over 5 weeks as detected with real-time RT-PCR. Accumulation of collagen II and aggrecan in hydrogel extracellular matrix was observed after 5 weeks in cell culture. Overall, our results indicate that genipin appeared to inhibit the inflammatory reaction observed 3 weeks after subcutaneous implantation of the fibrin into rats. Therefore, genipin cross-linked fibrin hydrogels can be used as cell-compatible tissue engineering scaffolds for articular cartilage regeneration, for utility in autologous treatments that eliminate the risk of tissue rejection and viral infection. | 19287127
 |
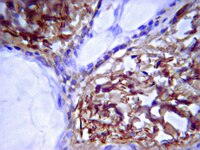
Discoidin domain receptor-1 deficiency attenuates atherosclerotic calcification and smooth muscle cell-mediated mineralization.
Ahmad PJ, Trcka D, Xue S, Franco C, Speer MY, Giachelli CM, Bendeck MP
The American journal of pathology
175
2686-96
2009
Show Abstract
Intimal calcification is a feature of advanced atherosclerotic disease that predicts a two- to eightfold increase in the risk of coronary events. Type I collagen promotes vascular smooth muscle cell-mediated calcification, although the mechanism by which this occurs is unknown. The discoidin domain receptor 1 (DDR1) is a collagen receptor that is emerging as a critical mediator of atherosclerosis. To determine whether DDR1 is involved in intimal calcification, we fed male Ddr1(-/-);Ldlr(-/-) and Ddr1(+/+);Ldlr(-/-) mice an atherogenic diet for 6, 12, or 24 weeks. DDR1 deficiency significantly reduced the calcium content of the aortic arch, and microcomputed tomography demonstrated a significant decrease in hydroxyapatite deposition after 24 weeks of atherogenic diet. Reduced calcification was correlated with decreases in macrophage accumulation and tumor necrosis factor alpha staining, suggesting that the reduction in calcification was in part due to decreased inflammation. The chondrogenic markers type II collagen, type X collagen, and Sox-9 were expressed within the mineralized foci. An in vitro assay performed with vascular smooth muscle cells revealed that DDR1 was required for cell-mediated calcification of the matrix, and Ddr1(+/+) smooth muscle cells expressed more alkaline phosphatase activity, whereas Ddr1(-/-) smooth muscle cells expressed elevated levels of mRNA for nucleotide pyrophosphatase phosphodiesterase 1, an inhibitor of tissue mineralization. Taken together, our results demonstrate that DDR1 mediates an important mechanism for atherosclerotic calcification. | 19893047
 |
Participation of collagen types I, III, IV, V, and fibronectin in the formation of villi fibrosis in human term placenta.
Rukosuev, V S, et al.
Acta Histochem., 89: 11-6 (1990)
1990
Show Abstract
The indirect immunofluorescence method was used to study the human term placenta in pathological pregnancy for the distribution of collagen types I, III, IV, V, and fibronectin in fibrosis stromatis villi. All collagen types and fibronectin were shown to participate in fibrosis villorum formation. Fibronectin was also detected in the fibrinoid that surrounded villi at stroma. The presence of free cytotrophoblast cells in the fibrinoid was accompanied by a noticeable increase in fibronectin fluorescence. A significant amount of collagen types IV and V and a less amount of collagen types I and III were identified. | 1705376
 |