Bevacizumab treatment induces metabolic adaptation toward anaerobic metabolism in glioblastomas.
Fack, F; Espedal, H; Keunen, O; Golebiewska, A; Obad, N; Harter, PN; Mittelbronn, M; Bähr, O; Weyerbrock, A; Stuhr, L; Miletic, H; Sakariassen, PØ; Stieber, D; Rygh, CB; Lund-Johansen, M; Zheng, L; Gottlieb, E; Niclou, SP; Bjerkvig, R
Acta neuropathologica
129
115-31
2015
Abstract anzeigen
Anti-angiogenic therapy in glioblastoma (GBM) has unfortunately not led to the anticipated improvement in patient prognosis. We here describe how human GBM adapts to bevacizumab treatment at the metabolic level. By performing (13)C6-glucose metabolic flux analysis, we show for the first time that the tumors undergo metabolic re-programming toward anaerobic metabolism, thereby uncoupling glycolysis from oxidative phosphorylation. Following treatment, an increased influx of (13)C6-glucose was observed into the tumors, concomitant to increased lactate levels and a reduction of metabolites associated with the tricarboxylic acid cycle. This was confirmed by increased expression of glycolytic enzymes including pyruvate dehydrogenase kinase in the treated tumors. Interestingly, L-glutamine levels were also reduced. These results were further confirmed by the assessment of in vivo metabolic data obtained by magnetic resonance spectroscopy and positron emission tomography. Moreover, bevacizumab led to a depletion in glutathione levels indicating that the treatment caused oxidative stress in the tumors. Confirming the metabolic flux results, immunohistochemical analysis showed an up-regulation of lactate dehydrogenase in the bevacizumab-treated tumor core as well as in single tumor cells infiltrating the brain, which may explain the increased invasion observed after bevacizumab treatment. These observations were further validated in a panel of eight human GBM patients in which paired biopsy samples were obtained before and after bevacizumab treatment. Importantly, we show that the GBM adaptation to bevacizumab therapy is not mediated by clonal selection mechanisms, but represents an adaptive response to therapy. | | | 25322816
 |
The changes of angiogenesis and immune cell infiltration in the intra- and peri-tumoral melanoma microenvironment.
Zidlik, V; Brychtova, S; Uvirova, M; Ziak, D; Dvorackova, J
International journal of molecular sciences
16
7876-89
2015
Abstract anzeigen
Malignant melanoma (MM) urgently needs identification of new markers with better predictive value than currently-used clinical and histological parameters. Cancer cells stimulate the formation of a specialized tumor microenvironment, which reciprocally affects uncontrolled proliferation and migration. However, this microenvironment is heterogeneous with different sub-compartments defined by their access to oxygen and nutrients. This study evaluated microvascular density (MVD), CD3+ lymphocytes (TILs) and FOXP3+ T-regulatory lymphocytes (Tregs) on formalin-fixed paraffin-embedded tissue sections using light microscopy. We analyzed 82 malignant melanomas, divided according to the AJCC TNM classification into four groups--pT1 (35), pT2 (17), pT3 (18) and pT4 (12)--and 25 benign pigmented nevi. All parameters were measured in both the central areas of tumors (C) and at their periphery (P). A marked increase in all parameters was found in melanomas compared to nevi (p = 0.0001). There was a positive correlation between MVD, TILs, FOXP3+ Tregs and the vertical growth phase. The results show that MVD, TILs and FOXP3+ Tregs substantially influence cutaneous melanoma microenvironment. We found significant topographic differences of the parameters between central areas of tumors and their boundaries. | | | 25913374
 |
Induced pluripotent stem cell-derived neuronal cells from a sporadic Alzheimer's disease donor as a model for investigating AD-associated gene regulatory networks.
Hossini, AM; Megges, M; Prigione, A; Lichtner, B; Toliat, MR; Wruck, W; Schröter, F; Nuernberg, P; Kroll, H; Makrantonaki, E; Zouboulis, CC; Zoubouliss, CC; Adjaye, J
BMC genomics
16
84
2015
Abstract anzeigen
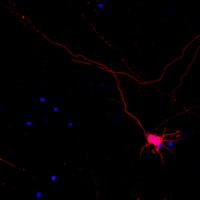
Alzheimer's disease (AD) is a complex, irreversible neurodegenerative disorder. At present there are neither reliable markers to diagnose AD at an early stage nor therapy. To investigate underlying disease mechanisms, induced pluripotent stem cells (iPSCs) allow the generation of patient-derived neuronal cells in a dish.In this study, employing iPS technology, we derived and characterized iPSCs from dermal fibroblasts of an 82-year-old female patient affected by sporadic AD. The AD-iPSCs were differentiated into neuronal cells, in order to generate disease-specific protein association networks modeling the molecular pathology on the transcriptome level of AD, to analyse the reflection of the disease phenotype in gene expression in AD-iPS neuronal cells, in particular in the ubiquitin-proteasome system (UPS), and to address expression of typical AD proteins. We detected the expression of p-tau and GSK3B, a physiological kinase of tau, in neuronal cells derived from AD-iPSCs. Treatment of neuronal cells differentiated from AD-iPSCs with an inhibitor of γ-secretase resulted in the down-regulation of p-tau. Transcriptome analysis of AD-iPS derived neuronal cells revealed significant changes in the expression of genes associated with AD and with the constitutive as well as the inducible subunits of the proteasome complex. The neuronal cells expressed numerous genes associated with sub-regions within the brain thus suggesting the usefulness of our in-vitro model. Moreover, an AD-related protein interaction network composed of APP and GSK3B among others could be generated using neuronal cells differentiated from two AD-iPS cell lines.Our study demonstrates how an iPSC-based model system could represent (i) a tool to study the underlying molecular basis of sporadic AD, (ii) a platform for drug screening and toxicology studies which might unveil novel therapeutic avenues for this debilitating neuronal disorder. | | | 25765079
 |
Rapid and Efficient Generation of Transgene-Free iPSC from a Small Volume of Cryopreserved Blood.
Zhou, H; Martinez, H; Sun, B; Li, A; Zimmer, M; Katsanis, N; Davis, EE; Kurtzberg, J; Lipnick, S; Noggle, S; Rao, M; Chang, S
Stem cell reviews
11
652-65
2015
Abstract anzeigen
Human peripheral blood and umbilical cord blood represent attractive sources of cells for reprogramming to induced pluripotent stem cells (iPSCs). However, to date, most of the blood-derived iPSCs were generated using either integrating methods or starting from T-lymphocytes that have genomic rearrangements thus bearing uncertain consequences when using iPSC-derived lineages for disease modeling and cell therapies. Recently, both peripheral blood and cord blood cells have been reprogrammed into transgene-free iPSC using the Sendai viral vector. Here we demonstrate that peripheral blood can be utilized for medium-throughput iPSC production without the need to maintain cell culture prior to reprogramming induction. Cell reprogramming can also be accomplished with as little as 3000 previously cryopreserved cord blood cells under feeder-free and chemically defined Xeno-free conditions that are compliant with standard Good Manufacturing Practice (GMP) regulations. The first iPSC colonies appear 2-3 weeks faster in comparison to previous reports. Notably, these peripheral blood- and cord blood-derived iPSCs are free of detectable immunoglobulin heavy chain (IGH) and T cell receptor (TCR) gene rearrangements, suggesting they did not originate from B- or T- lymphoid cells. The iPSCs are pluripotent as evaluated by the scorecard assay and in vitro multi lineage functional cell differentiation. Our data show that small volumes of cryopreserved peripheral blood or cord blood cells can be reprogrammed efficiently at a convenient, cost effective and scalable way. In summary, our method expands the reprogramming potential of limited or archived samples either stored at blood banks or obtained from pediatric populations that cannot easily provide large quantities of peripheral blood or a skin biopsy. | | | 25951995
 |
Inhibition of Excessive Monoamine Oxidase A/B Activity Protects Against Stress-induced Neuronal Death in Huntington Disease.
Ooi, J; Hayden, MR; Pouladi, MA
Molecular neurobiology
52
1850-61
2015
Abstract anzeigen
Monoamine oxidases (MAO) are important components of the homeostatic machinery that maintains the levels of monoamine neurotransmitters, including dopamine, in balance. Given the imbalance in dopamine levels observed in Huntington disease (HD), the aim of this study was to examine MAO activity in a mouse striatal cell model of HD and in human neural cells differentiated from control and HD patient-derived induced pluripotent stem cell (hiPSC) lines. We show that mouse striatal neural cells expressing mutant huntingtin (HTT) exhibit increased MAO expression and activity. We demonstrate using luciferase promoter assays that the increased MAO expression reflects enhanced epigenetic activation in striatal neural cells expressing mutant HTT. Using cellular stress paradigms, we further demonstrate that the increase in MAO activity in mutant striatal neural cells is accompanied by enhanced susceptibility to oxidative stress and impaired viability. Treatment of mutant striatal neural cells with MAO inhibitors ameliorated oxidative stress and improved cellular viability. Finally, we demonstrate that human HD neural cells exhibit increased MAO-A and MAO-B expression and activity. Altogether, this study demonstrates abnormal MAO expression and activity and suggests a potential use for MAO inhibitors in HD. | | | 25398695
 |
Early gestation chorionic villi-derived stromal cells for fetal tissue engineering.
Lankford, L; Selby, T; Becker, J; Ryzhuk, V; Long, C; Farmer, D; Wang, A
World journal of stem cells
7
195-207
2015
Abstract anzeigen
To investigate the potential for early gestation placenta-derived mesenchymal stromal cells (PMSCs) for fetal tissue engineering.PMSCs were isolated from early gestation chorionic villus tissue by explant culture. Chorionic villus sampling (CVS)-size tissue samples (mean = 35.93 mg) were used to test the feasibility of obtaining large cell numbers from CVS within a clinically relevant timeframe. We characterized PMSCs isolated from 6 donor placentas by flow cytometry immunophenotyping, multipotency assays, and through immunofluorescent staining. Protein secretion from PMSCs was examined using two cytokine array assays capable of probing for over 70 factors in total. Delivery vehicle compatibility of PMSCs was determined using three common scaffold systems: fibrin glue, collagen hydrogel, and biodegradable nanofibrous scaffolds made from a combination of polylactic acid (PLA) and poly(lactic-co-glycolic acid) (PLGA). Viral transduction of PMSCs was performed using a Luciferase-GFP-containing lentiviral vector and efficiency of transduction was tested by fluorescent microscopy and flow cytometry analysis.We determined that an average of 2.09 × 10(6) (SD ± 8.59 × 10(5)) PMSCs could be obtained from CVS-size tissue samples within 30 d (mean = 27 d, SD ± 2.28), indicating that therapeutic numbers of cells can be rapidly expanded from very limited masses of tissue. Immunophenotyping by flow cytometry demonstrated that PMSCs were positive for MSC markers CD105, CD90, CD73, CD44, and CD29, and were negative for hematopoietic and endothelial markers CD45, CD34, and CD31. PMSCs displayed trilineage differentiation capability, and were found to express developmental transcription factors Sox10 and Sox17 as well as neural-related structural proteins NFM, Nestin, and S100β. Cytokine arrays revealed a robust and extensive profile of PMSC-secreted cytokines and growth factors, and detected 34 factors with spot density values exceeding 10(3). Detected factors had widely diverse functions that include modulation of angiogenesis and immune response, cell chemotaxis, cell proliferation, blood vessel maturation and homeostasis, modulation of insulin-like growth factor activity, neuroprotection, extracellular matrix degradation and even blood coagulation. Importantly, PMSCs were also determined to be compatible with both biological and synthetic material-based delivery vehicles such as collagen and fibrin hydrogels, and biodegradable nanofiber scaffolds made from a combination of PLA and PLGA. Finally, we demonstrated that PMSCs can be efficiently transduced (greater than 95%) with a Luciferase-GFP-containing lentiviral vector for future in vivo cell tracking after transplantation.Our findings indicate that PMSCs represent a unique source of cells that can be effectively utilized for in utero cell therapy and tissue engineering. | | | 25621120
 |
Inhibitor of DNA Binding 4 (ID4) is highly expressed in human melanoma tissues and may function to restrict normal differentiation of melanoma cells.
Peretz, Y; Wu, H; Patel, S; Bellacosa, A; Katz, RA
PloS one
10
e0116839
2015
Abstract anzeigen
Melanoma tissues and cell lines are heterogeneous, and include cells with invasive, proliferative, stem cell-like, and differentiated properties. Such heterogeneity likely contributes to the aggressiveness of the disease and resistance to therapy. One model suggests that heterogeneity arises from rare cancer stem cells (CSCs) that produce distinct cancer cell lineages. Another model suggests that heterogeneity arises through reversible cellular plasticity, or phenotype-switching. Recent work indicates that phenotype-switching may include the ability of cancer cells to dedifferentiate to a stem cell-like state. We set out to investigate the phenotype-switching capabilities of melanoma cells, and used unbiased methods to identify genes that may control such switching. We developed a system to reversibly synchronize melanoma cells between 2D-monolayer and 3D-stem cell-like growth states. Melanoma cells maintained in the stem cell-like state showed a striking upregulation of a gene set related to development and neural stem cell biology, which included SRY-box 2 (SOX2) and Inhibitor of DNA Binding 4 (ID4). A gene set related to cancer cell motility and invasiveness was concomitantly downregulated. Intense and pervasive ID4 protein expression was detected in human melanoma tissue samples, suggesting disease relevance for this protein. SiRNA knockdown of ID4 inhibited switching from monolayer to 3D-stem cell-like growth, and instead promoted switching to a highly differentiated, neuronal-like morphology. We suggest that ID4 is upregulated in melanoma as part of a stem cell-like program that facilitates further adaptive plasticity. ID4 may contribute to disease by preventing stem cell-like melanoma cells from progressing to a normal differentiated state. This interpretation is guided by the known role of ID4 as a differentiation inhibitor during normal development. The melanoma stem cell-like state may be protected by factors such as ID4, thereby potentially identifying a new therapeutic vulnerability to drive differentiation to the normal cell phenotype. | | | 25642713
 |
17β-estradiol protects human eyelid-derived adipose stem cells against cytotoxicity and increases transplanted cell survival in spinal cord injury.
Zhou, J; Lu, P; Ren, H; Zheng, Z; Ji, J; Liu, H; Jiang, F; Ling, S; Heng, BC; Hu, X; Ouyang, H
Journal of cellular and molecular medicine
18
326-43
2014
Abstract anzeigen
Stem cell transplantation represents a promising strategy for the repair of spinal cord injury (SCI). However, the low survival rate of the grafted cells is a major obstacle hindering clinical success because of ongoing secondary injury processes, which includes excitotoxicity, inflammation and oxidative stress. Previous studies have shown that 17b-estradiol (E2) protects several cell types against cytotoxicity. Thus, we examined the effects of E2 on the viability of human eyelid adipose-derived stem cells (hEASCs) in vitro with hydrogen peroxide (H₂O₂)-induced cell model and in vivo within a rat SCI model. Our results showed that E2 protected hEASCs against H₂O₂-induced cell death in vitro, and enhanced the survival of grafted hEASCs in vivo by reducing apoptosis. Additionally, E2 also enhanced the secretion of growth factors by hEASCs, thereby making the local microenvironment more conducive for tissue regeneration. Overall, E2 administration enhanced the therapeutic efficacy of hEASCs transplantation and facilitated motor function recovery after SCI. Hence, E2 administration may be an intervention of choice for enhancing survival of transplanted hEASCs after SCI. | Immunocytochemistry | Human | 24373095
 |
Comparison of the molecular profiles of human embryonic and induced pluripotent stem cells of isogenic origin.
Mallon, BS; Hamilton, RS; Kozhich, OA; Johnson, KR; Fann, YC; Rao, MS; Robey, PG
Stem cell research
12
376-86
2014
Abstract anzeigen
Many studies have compared the genetic and epigenetic profiles of human induced pluripotent stem cells (hiPSCs) to human embryonic stem cells (hESCs) and yet the picture remains unclear. To address this, we derived a population of neural precursor cells (NPCs) from the H1 (WA01) hESC line and generated isogenic iPSC lines by reprogramming. The gene expression and methylation profile of three lines were compared to the parental line and intermediate NPC population. We found no gene probe with expression that differed significantly between hESC and iPSC samples under undifferentiated or differentiated conditions. Analysis of the global methylation pattern also showed no significant difference between the two PSC populations. Both undifferentiated populations were distinctly different from the intermediate NPC population in both gene expression and methylation profiles. One point to note is that H1 is a male line and so extrapolation to female lines should be cautioned. However, these data confirm our previous findings that there are no significant differences between hESCs and hiPSCs at the gene expression or methylation level. | | | 24374290
 |
Generation of iPS Cells from Human Hair Follice Dermal Papilla Cells.
Muchkaeva, IA; Dashinimaev, EB; Artyuhov, AS; Myagkova, EP; Vorotelyak, EA; Yegorov, YY; Vishnyakova, KS; Kravchenko, IE; Chumakov, PM; Terskikh, VV; Vasiliev, AV
Acta naturae
6
45-53
2014
Abstract anzeigen
Dermal papilla (DP) cells are unique regional stem cells of the skin that induce formation of a hair follicle and its regeneration cycle. DP are multipotent stem cells; therefore we supposed that the efficiency of DPC reprogramming could exceed that of dermal fibroblasts reprogramming. We generated induced pluripotent stem cells from human DP cells using lentiviral transfection with Oct4, Sox2, Klf4, and c-Myc, and cultivation of cells both in a medium supplemented with valproic acid and at a physiological level of oxygen (5%). The efficiency of DP cells reprogramming was ~0.03%, while the efficiency of dermal fibroblast reprogramming under the same conditions was ~0.01%. Therefore, we demonstrated the suitability of DP cells as an alternative source of iPS cells. | | | 24772326
 |