Bacterial induction of Snail1 contributes to blood-brain barrier disruption.
Kim, BJ; Hancock, BM; Bermudez, A; Del Cid, N; Reyes, E; van Sorge, NM; Lauth, X; Smurthwaite, CA; Hilton, BJ; Stotland, A; Banerjee, A; Buchanan, J; Wolkowicz, R; Traver, D; Doran, KS
The Journal of clinical investigation
125
2473-83
2015
Abstract anzeigen
Bacterial meningitis is a serious infection of the CNS that results when blood-borne bacteria are able to cross the blood-brain barrier (BBB). Group B Streptococcus (GBS) is the leading cause of neonatal meningitis; however, the molecular mechanisms that regulate bacterial BBB disruption and penetration are not well understood. Here, we found that infection of human brain microvascular endothelial cells (hBMECs) with GBS and other meningeal pathogens results in the induction of host transcriptional repressor Snail1, which impedes expression of tight junction genes. Moreover, GBS infection also induced Snail1 expression in murine and zebrafish models. Tight junction components ZO-1, claudin 5, and occludin were decreased at both the transcript and protein levels in hBMECs following GBS infection, and this repression was dependent on Snail1 induction. Bacteria-independent Snail1 expression was sufficient to facilitate tight junction disruption, promoting BBB permeability to allow bacterial passage. GBS induction of Snail1 expression was dependent on the ERK1/2/MAPK signaling cascade and bacterial cell wall components. Finally, overexpression of a dominant-negative Snail1 homolog in zebrafish elevated transcription of tight junction protein-encoding genes and increased zebrafish survival in response to GBS challenge. Taken together, our data support a Snail1-dependent mechanism of BBB disruption and penetration by meningeal pathogens. | | 25961453
 |
Disrupted tight junctions in the small intestine of cystic fibrosis mice.
De Lisle, RC
Cell and tissue research
355
131-42
2014
Abstract anzeigen
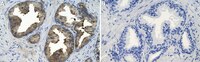
The tight junction (TJ) is the major determinant of paracellular permeability, which in the gut protects the body from entry of harmful substances such as microbial components. In cystic fibrosis (CF), there is increased permeability of the small intestine both in humans and in CF mice. To gain insight into the mechanisms of increased intestinal permeability in CF, I analyze the composition of the TJ in a cystic fibrosis transmembrane conductance regulator (Cftr) knockout mouse model. Significant changes in TJ gene expression in the CF intestine were found for Cldn1, Cldn7, Cldn8 and Pmp22, which were expressed at lower levels and Cldn2 that was expressed at a higher level. Protein levels of claudin-2 were increased in the CF intestine as compared to wild-type, while other TJ proteins were not significantly different. In the villus epithelium of the CF intestine, all TJ components analyzed were mislocalized to the basal cytoplasm and showed varying degrees of loss from the TJ and apico-lateral surfaces. The pore-forming claudin-2 in the CF intestine showed more intense staining but was correctly localized to the TJ, principally in the crypts that are enlarged in CF. The cytokine TNFα, known to affect TJ, was elevated to 160% of wild-type in the CF intestine. In summary, there is a dramatic redistribution of claudin proteins from the TJ/lateral membrane to the basal cytoplasm of the villus epithelium in the CF intestine. These changes in TJ protein localization in CF are likely to be involved in the increased permeability of the CF small intestine to macromolecules and TNFα may be a causative factor. | | 24169862
 |
Cranial irradiation alters the brain's microenvironment and permits CCR2+ macrophage infiltration.
Morganti, JM; Jopson, TD; Liu, S; Gupta, N; Rosi, S
PloS one
9
e93650
2014
Abstract anzeigen
Therapeutic irradiation is commonly used to treat primary or metastatic central nervous system tumors. It is believed that activation of neuroinflammatory signaling pathways contributes to the development of common adverse effects, which may ultimately contribute to cognitive dysfunction. Recent studies identified the chemokine (C-C motif) receptor (CCR2), constitutively expressed by cells of the monocyte-macrophage lineage, as a mediator of cognitive impairments induced by irradiation. In the present study we utilized a unique reporter mouse (CCR2(RFP/+)CX3CR1(GFP/+)) to accurately delineate the resident (CX3CR1+) versus peripheral (CCR2+) innate immune response in the brain following cranial irradiation. Our results demonstrate that a single dose of 10Gy cranial γ-irradiation induced a significant decrease in the percentage of resident microglia, while inducing an increase in the infiltration of peripherally derived CCR2+ macrophages. Although reduced in percentage, there was a significant increase in F4/80+ activated macrophages in irradiated animals compared to sham. Moreover, we found that there were altered levels of pro-inflammatory cytokines, chemokines, adhesion molecules, and growth factors in the hippocampi of wild type irradiated mice as compared to sham. All of these molecules are implicated in the recruitment, adhesion, and migration of peripheral monocytes to injured tissue. Importantly, there were no measureable changes in the expression of multiple markers associated with blood-brain barrier integrity; implicating the infiltration of peripheral CCR2+ macrophages may be due to inflammatory induced chemotactic signaling. Cumulatively, these data provide evidence that therapeutic levels of cranial radiation are sufficient to alter the brain's homeostatic balance and permit the influx of peripherally-derived CCR2+ macrophages as well as the regional susceptibility of the hippocampal formation to ionizing radiation. | Western Blotting | 24695541
 |