The role of transforming growth factor beta isoforms in tendon-to-bone healing.
H Mike Kim,Leesa M Galatz,Rosalina Das,Necat Havlioglu,Stefan Y Rothermich,Stavros Thomopoulos
Connective tissue research
52
2011
Show Abstract
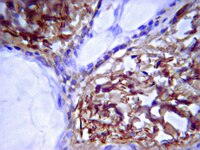
The purpose of this study was to examine the role of two of the three transforming growth factor beta (TGF-β) isoforms at the healing tendon-to-bone insertion. The supraspinatus tendons of 64 rats were transected at their bony insertions and repaired to the humeral head. One shoulder of each rat received an osmotic pump for sustained delivery of the following factors at the repair site: (1) TGF-β1 and neutralizing antibodies to TGF-β2 and 3 (TGF-β1 group), (2) TGF-β3 and neutralizing antibodies to TGF-β1 and 2 (TGF-β3 group), (3) neutralizing antibodies to TGF-β1, 2, and 3 (anti-TGF-β group), and (4) saline (saline group). The contralateral shoulders received saline to serve as paired controls. The repairs were evaluated at multiple time points postmortem using histology-based assays and biomechanical testing. Treated shoulders in the TGF-β1 group showed increased type III collagen production compared to the paired control shoulders, indicative of a scar-mediated response. There was a trend toward reduced mechanical properties in the TGF-β1 group, but these changes did not reach statistical significance. The anti-TGF-β group showed no difference in tissue volume, but significantly inferior mechanical properties, compared to the paired control shoulders. The TGF-β3 group did not show any differences compared to the paired control shoulders. Although TGF-β isoforms play important roles in tendon-to-bone development and healing, application of exogenous TGF-β isoforms and neutralizing antibodies to the subacromial space using osmotic pumps did not improve supraspinatus tendon-to-bone healing. | 20615095
 |
Fibrin Glues in Combination with Mesenchymal Stem cells to Develop a Tissue-engineered Cartilage Substitute.
Ahmed TA, Giulivi A, Griffith M, Hincke MT
Tissue Eng Part A
2010
Show Abstract
Damage of cartilage due to traumatic or pathological conditions results in disability and severe pain. Regenerative medicine, using tissue engineering-based constructs to enhance cartilage repair by mobilizing chondrogenic cells, is a promising approach for restoration of structure and function. Fresh fibrin (FG) and platelet-rich fibrin (PR-FG) glues produced by the CryoSeal(R) FS System, in combination with human bone marrow-derived mesenchymal stem cells (BM-hMSCs), were evaluated in this study. We additionally tested the incorporation of heparin-based delivery system (HBDS) into these scaffolds to immobilize endogenous growth factors as well as exogenous TGF-beta2. Strongly CD90+ and CD105+ hMSCs were encapsulated into FG and PR-FG with and without HBDS. Encapsulation of hMSCs in PR-FG led to increased expression of collagen II gene at 2.5 weeks, however, no difference was observed between FG and PR-FG at 5 weeks. The incorporation of HBDS prevented the enhancement of collagen II gene expression. BM-hMSCs in FG initially displayed enhanced aggrecan gene expression and increased accumulation of Alcian blue-positive extracellular matrix (ECM); incorporation of HBDS into these glues did not improve aggrecan gene expression and ECM accumulation. The most significant effect on cartilage marker gene expression and accumulation was observed after encapsulation of hMSCs in FG. We conclude that fibrin glue is more promising than platelet-rich fibrin glue as a scaffold for chondrogenic differentiation of hMSCs; however, immobilization of growth factors inside these fibrin scaffolds with the HBDS system has a negative impact on this process. In addition, BM-hMSCs are valid and potentially superior alternatives to chondrocytes for tissue engineering of articular cartilage. | 20799906
 |
Characterization and inhibition of fibrin hydrogel-degrading enzymes during development of tissue engineering scaffolds.
Tamer A E Ahmed,May Griffith,Max Hincke
Tissue engineering
13
2007
Show Abstract
The goal of articular cartilage tissue engineering is to provide cartilaginous constructs to replace abnormal cartilage. We have evaluated the chondroprogenitor clonal cell line RCJ3.1C5.18 (C5.18) as a model to guide the development of appropriate scaffolds for tissue engineering. Rapid degradation of fibrin hydrogels was observed after encapsulation of C5.18 cells. The enzymes responsible for this fibrin gel breakdown were characterized to control their activity and regulate gel stability. Western blotting, confirming zymography, revealed bands due to matrix metalloproteinases (MMP-2, MMP-3) that are secreted concomitantly with fibrin hydrogels breakdown. High plasmin activity was detected in conditioned media during hydrogel breakdown but not in the confluent cells before encapsulation. Reverse transcriptase polymerase chain reaction indicated the expression of MMP-2, -3, and -9 and plasminogen in the cells. MMP-9 was 100 times higher at day 1, whereas MMP-2 started to increase and reached its maximum level by day 7. Aprotinin, a known serine protease inhibitor, and galardin (GM6001), a potent MMP inhibitor, in combination or separately, prevented the breakdown of fibrin-C5.18 hydrogels, whereas only the combination of both promoted the accumulation of extracellular matrix. These findings suggest that plasmin and MMPs contribute independently to fibrin hydrogel breakdown, but that either enzyme can achieve extracellular matrix breakdown. | 17518706
 |